Oesophagal varices are submucosal distal oesophagal veins that connect the portal circulation and systemic circulation, which are dilated due to portal hypertension, most commonly because of cirrhosis. Variceal haemorrhage is the most common fatal complication of cirrhosis.
Clinical Features
- Characteristically massive upper GI bleeding
- Other s/s of portal hypertension
Prognosis
- 30% of all patients with cirrhosis have varices. Develop at a rate of 5-15% per year.
- 30% of patients with varices will develop bleeding.
- 30% mortality associated with each bleed.
Risk Factors for bleeding
- Location of varices – highest risk in gastroesophageal junction varices.
- Size of varices
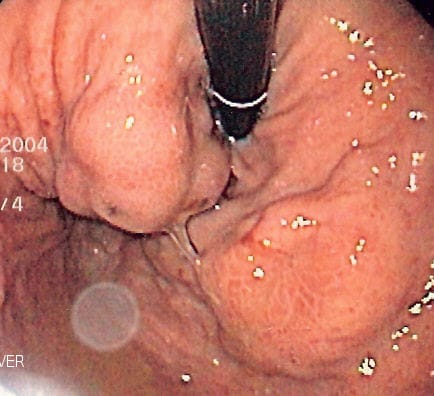
- Endoscopic characteristics – red wale marks
- The severity of cirrhosis – a higher Child-Pugh/MELD score
- Tense ascites
- High variceal pressure
Diagnosis
- Endoscopy – Invx of choice
Management of bleeding
- Resuscitation – Maintain intravascular volume with fluid/blood products.
- Vasoconstriction: Terlipressin, octreotide, somatostatin
- Endoscopic management: Ligation/sclerotherapy
- Balloon tamponade – interim measure awaiting endoscopy
- TIPSS
- Prophylactic antibiotics to reduce incidence of spontaneous bacterial peritonitis – oral ciprofloxacin or IV cephalosporin.
- PPIs – To prevent peptic ulcers.
Prevention of re-bleeding
- Beta blockade- propranolol, nadolol
- Repeated variceal ligation until all varices are obliterated.












