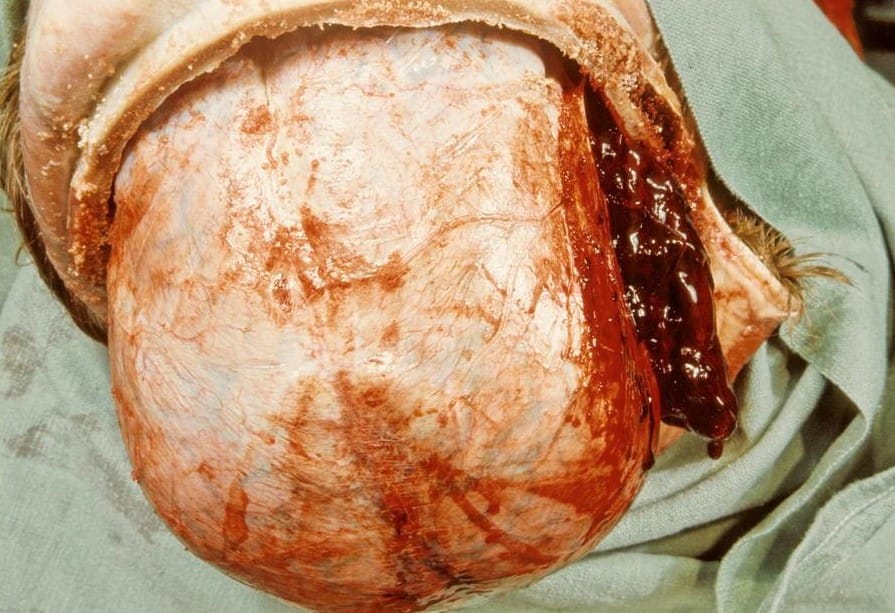
Epidural hematomas are located in the space between the dura and the skull
Most cases are due to head trauma following traffic accidents, falls, and assaults. The majority are due to trauma to the skull base, causing tearing of the middle meningeal artery, which causes bleeding in the middle cranial fossa
It may occasionally be found in the anterior cranial fossa due to the rupture of the anterior meningeal artery
Skull fractures coexist in 75 to 90% of cases
More common in ages 20 to 30, rare in older individuals
Nontraumatic EDH is rare. It may be due to;
- Infection
- Neurosurgical procedures
- Epidural abscess
- Pregnancy
- Hemodialysis
- Paget disease of the skull, etc
Clinical presentation;
- Coma with severe head trauma
- Momentary loss of consciousness in lesser injury.
- “Lucid interval” is typical; consciousness is recovered, followed by deterioration. The deterioration is characterized by drowsiness, confusion, vomiting, aphasia, seizures, and hemiparesis
- Hematoma expansion causes raised ICP with an ipsilateral dilated pupil or the Cushing reflex( hypertension, bradycardia, and respiratory irregularities). This will lead to herniation and death unless immediate decompression is done
- Cortical blindness may occur with posterior fossa EDH
Diagnosis
1. Head CT- most are identifiable
- Lens-shaped or biconvex pattern because it’s limited by firm dural attachments and cranial sutures
- Hematoma volume influences management. The volume can be estimated from the CT scan
2. Brain MRI- it is more sensitive though less widely used. It is more useful in an EDH at the vertex
3. Angiography- to evaluate EDH, e.g., from a dural AV fistula
Management
- It is a neurological emergency.
- ABCDE approach to stabilize the patient, rule out any skull fractures on examination and imaging
- Reverse anticoagulation
- Select patients with a small volume EDH and good clinical condition can be managed non-operatively with close observation and serial brain imaging.
- Glucocorticoid use is not indicated. It has been associated with increased acute mortality.
Indications for surgery;
- GCS<9 and pupillary abnormalities
- Hematoma volume>30 ml
- Focal signs attributable to the EDH
- Hematoma expansion causing elevated ICP or neurologic deterioration
Surgical technique- craniotomy with hematoma evacuation
- Craniectomy if there’s significant cerebral edema or midline shift
-Middle meningeal artery embolization to stabilize bleeding and avoid open surgery for some patients with small EDH
-Surgery should be performed within one to two hours after head trauma or onset of neurologic deterioration in comatose patients
Prognosis
Generally good after surgery
Unfavorable outcomes;
- Low GCS at presentation
- Older age
- Pupillary abnormalities
- Coagulopathy or leucocytosis
- A longer interval between neurologic deterioration and surgery
- Postoperative elevated ICP
- Hematoma volume >30 ml
- Midline shift
- Mixed density clot, indicating acute bleeding
- Presence of intracranial hematomas, contusions, subarachnoid hemorrhage, or diffuse brain swelling












