Gastroschisis is a congenital defect of the abdominal wall characterized by the extrusion of abdominal organs, typically the intestines, through an opening in the abdominal wall, usually located to the right of the umbilical cord. Unlike omphalocele, in gastroschisis, the protruding organs are not covered by a protective membrane (sac), leading to direct exposure to the amniotic fluid during fetal development.
Pathophysiology
The exact cause of gastroschisis is not fully understood, but the condition is thought to result from a failure in the formation of the anterior abdominal wall during embryonic development. Several mechanisms have been proposed:
- Vascular Disruption Hypothesis: A disruption in the blood supply to the developing abdominal wall may lead to weakness or defects in the area, allowing for herniation.
- Abnormal Involution of the Right Umbilical Vein: In some cases, the right umbilical vein fails to regress normally, causing incomplete closure of the abdominal wall.
- Genetic and Environmental Factors: Although there is no clear genetic link, some studies suggest that genetic predispositions, combined with environmental factors (e.g., maternal smoking, young maternal age), may contribute to the development of gastroschisis.
Epidemiology
- Incidence: The estimated incidence is approximately 4-5 per 10,000 live births. The prevalence has been increasing over the past few decades.
- Age: It is a congenital condition detected prenatally or at birth.
- Gender: More common in males than females.
- Risk Factors:
- Young Maternal Age: Mothers under the age of 20 have a higher risk.
- Maternal Smoking and Drug Use: Especially recreational drugs such as cocaine or methamphetamines.
- Inadequate Prenatal Care: Associated with higher rates of gastroschisis.
- Low Socioeconomic Status: May be linked with other risk factors like inadequate nutrition or exposure to teratogens.
Clinical Features
- Prenatal Diagnosis:
- Ultrasound Findings: Gastroschisis can be detected on a prenatal ultrasound as early as the first or second trimester. The ultrasound will show loops of bowel floating freely in the amniotic fluid, to the right of the umbilical cord insertion site.
- Elevated Maternal Serum Alpha-Fetoprotein (MSAFP): A higher than normal level of MSAFP may be detected in maternal blood screening, indicating a possible abdominal wall defect.
- Neonatal Presentation:
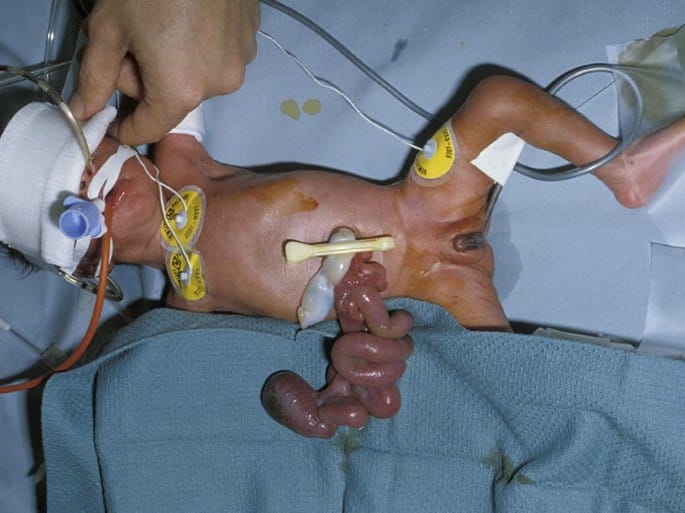
- Extruded Abdominal Contents: At birth, the intestines and occasionally other organs such as the stomach or liver are visible outside the abdomen.
- Inflamed and Edematous Bowel: Due to prolonged exposure to amniotic fluid, which can irritate and thicken the bowel wall.
- No Protective Sac: Unlike omphalocele, there is no peritoneal or amniotic sac covering the herniated organs.
Complications
Gastroschisis can be associated with a variety of complications, both prenatally and postnatally:
- Prenatal Complications:
- Intrauterine Growth Restriction (IUGR): Commonly observed in fetuses with gastroschisis.
- Preterm Delivery: Increased risk due to maternal complications or spontaneous preterm labor.
- Bowel Damage: Exposure to amniotic fluid can cause bowel inflammation, thickening, or damage, leading to intestinal dysfunction.
- Postnatal Complications:
- Malrotation: Abnormal twisting of the intestines, often present due to abnormal development.
- Short Bowel Syndrome: Resulting from extensive bowel damage or the need for surgical resection of non-viable segments.
- Feeding Intolerance and Prolonged Ileus: Delayed return of normal bowel function after surgery.
- Necrotizing Enterocolitis (NEC): A severe gastrointestinal disease that can occur after birth in neonates with gastroschisis.
- Sepsis: Increased risk of infection due to exposure of the abdominal contents.
Diagnostic Evaluation
- Prenatal Ultrasound: The primary tool for diagnosing gastroschisis. Serial ultrasounds are often performed to monitor fetal growth, bowel condition, and amniotic fluid levels.
- Magnetic Resonance Imaging (MRI): Occasionally used to obtain a more detailed evaluation of the bowel and other organs.
- Amniocentesis: May be performed if there is suspicion of other anomalies or genetic conditions, although gastroschisis itself is usually not associated with chromosomal abnormalities.
Management
The management of gastroschisis involves both prenatal planning and postnatal surgical correction.
- Prenatal Management:
- Frequent Monitoring: Regular ultrasounds to monitor fetal growth and amniotic fluid levels. Some cases may require more frequent visits to assess the condition of the bowel.
- Maternal Nutrition: Optimizing maternal nutrition may help improve fetal growth.
- Planned Delivery: Delivery is often planned at a specialized center equipped to handle high-risk neonates and pediatric surgical interventions. Delivery typically occurs between 37-39 weeks to reduce the risk of fetal bowel damage or intrauterine complications.
- Postnatal Management
Managing a newborn with gastroschisis requires immediate and carefully coordinated care to protect the exposed bowel and prepare the infant for surgical correction. Here’s a step-by-step guide on what to do after birth:
- Initial Stabilization and Resuscitation:
- Warm the Baby: Place the newborn in a warm environment, such as a radiant warmer, to maintain body temperature. Neonates with gastroschisis are at increased risk of hypothermia due to heat loss from the exposed organs.
- Airway and Breathing Assessment: Ensure that the baby’s airway is clear, and monitor breathing. Oxygen supplementation may be needed if there is respiratory distress.
- Circulation: Check heart rate, blood pressure, and capillary refill. Start intravenous (IV) access for fluid administration.
- Protection of the Exposed Bowel:
- Cover the Exposed Intestines: The exposed bowel should be immediately covered with sterile, saline-soaked gauze to keep it moist. The gauze helps prevent fluid loss and minimizes the risk of drying out and damage to the bowel.
- Wrap in a Plastic Covering or Silo Bag: Cover the moist gauze and the exposed bowel with a sterile, transparent plastic wrap or preformed silo bag. This helps reduce heat loss, prevents contamination, and minimizes fluid and electrolyte imbalance.
- Intravenous Fluid and Electrolyte Management:
- Administer IV Fluids: Start IV fluids to maintain hydration and electrolyte balance, as newborns with gastroschisis can lose a significant amount of fluid from the exposed bowel.
- Monitor Electrolytes: Regularly check blood electrolyte levels (sodium, potassium, calcium) and blood glucose, and adjust the IV fluids accordingly.
- Gastrointestinal Decompression:
- Place a Nasogastric (NG) Tube: Insert an NG tube to decompress the stomach and prevent distention. The tube should be connected to low, intermittent suction to drain gastric secretions.
- Monitoring and Supportive Care:
- Vital Signs Monitoring: Continuous monitoring of heart rate, respiratory rate, blood pressure, and oxygen saturation.
- Prevent Infection: Administer broad-spectrum antibiotics prophylactically to reduce the risk of sepsis, as the bowel is exposed to potential contaminants.
- Consultation with a Pediatric Surgeon:
- Surgical Team Involvement: Notify the pediatric surgical team immediately for assessment and planning of the surgical repair.
- Decide on Primary or Staged Closure: The surgical team will evaluate the bowel for signs of inflammation, damage, or ischemia and decide whether to perform primary closure (directly closing the abdominal defect) or staged repair using a silo.
- Surgical Intervention:
- Primary Closure: If the abdominal defect is small, the bowel is not excessively swollen, and the abdominal cavity can accommodate the reduced bowel without compromising breathing or circulation, the surgeon may perform primary closure.
- Staged Reduction (Silo Technique): If the bowel is too swollen or the abdominal cavity is too small for primary closure, a silo is placed over the exposed bowel. The silo allows for gradual reduction of the bowel back into the abdomen over several days. Once fully reduced, the defect is surgically closed.

- Postoperative Care:
- Continue IV Fluids and Electrolytes: Maintain IV fluid support, and continue monitoring electrolytes.
- Parenteral Nutrition (TPN): Start total parenteral nutrition (TPN) to provide essential nutrients since enteral feeding will not be possible initially.
- Pain Management: Provide appropriate pain relief with analgesics.
- Gradual Introduction of Enteral Feeding:
- Start Feeding Slowly: Once bowel function returns (evidenced by bowel sounds or passage of stool), introduce small amounts of breast milk or formula.
- Increase Feeding Gradually: Gradually increase the volume and frequency of feeds as tolerated, while monitoring for signs of feeding intolerance, such as vomiting or abdominal distension.
- Monitoring for Complications:
- Watch for Signs of Complications: Monitor for potential postoperative issues like necrotizing enterocolitis (NEC), bowel obstruction, or sepsis.
- Evaluate Bowel Function Regularly: Assess for feeding intolerance, growth, and signs of malabsorption.
- Long-Term Follow-Up:
- Nutritional Support: Consult with a dietitian for ongoing nutritional needs, especially if there is residual bowel dysfunction.
- Growth and Development Assessment: Monitor growth milestones and development to identify any delays.
- Psychosocial Support for Parents: Provide education and support to the family, addressing concerns about prognosis, future surgeries (if needed), and feeding strategies.
Prognosis
- Survival Rate: With modern surgical techniques and neonatal care, the survival rate for gastroschisis is over 90%. However, long-term morbidity can vary depending on the extent of bowel damage or other complications.
- Long-Term Outcomes: Many children lead normal lives after successful repair, but some may experience feeding difficulties, growth delays, or require long-term nutritional support if significant bowel damage occurred.
Follow-Up and Monitoring
- Nutritional Support: Regular follow-up with a pediatric nutritionist is often needed for children with feeding difficulties or short bowel syndrome.
- Growth Monitoring: Children with a history of gastroschisis may be at risk for growth retardation and should have their growth and development regularly assessed.
- Bowel Function Assessment: Evaluating for potential long-term issues such as constipation, diarrhea, or malabsorption.












