Cholelithiasis refers to the presence of gallstones in the gallbladder. It is more common in females than in males.
STONE COMPOSITION AND PATHOPHYSIOLOGY
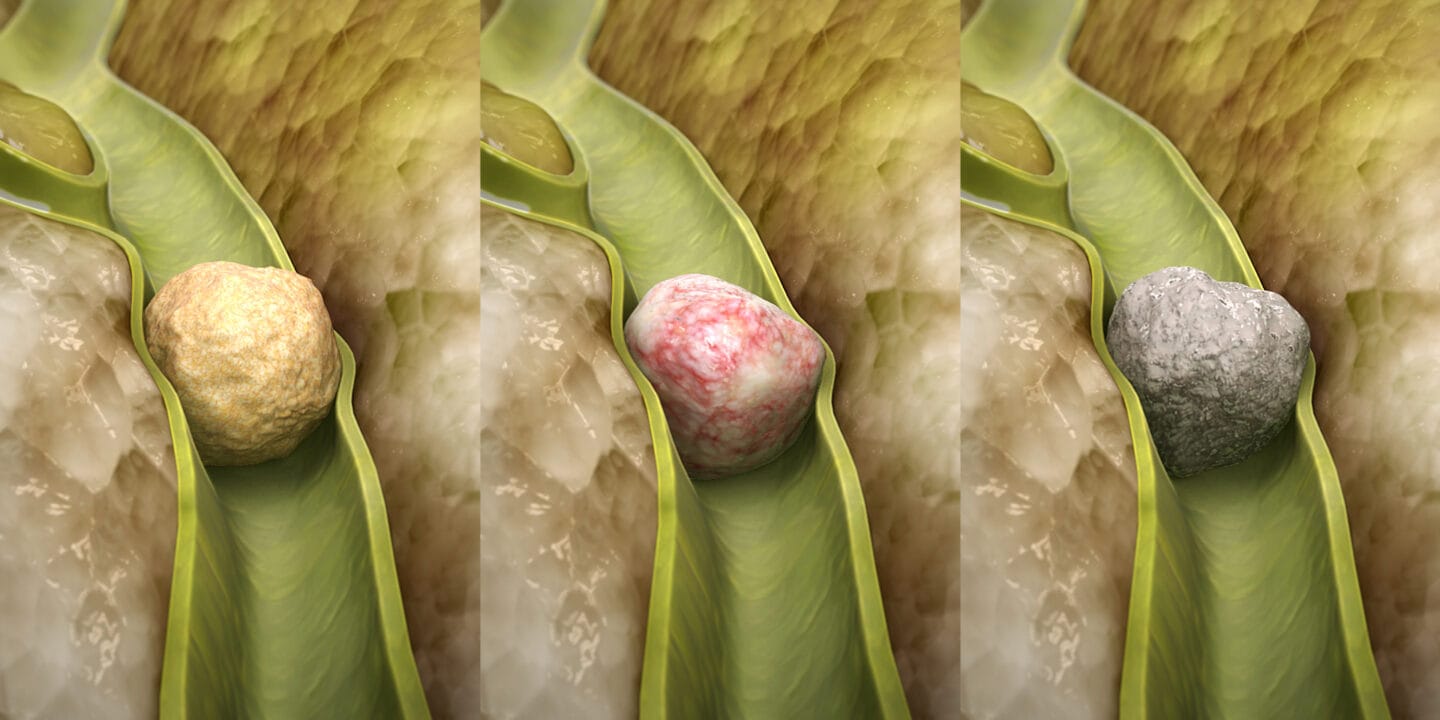
Cholesterol gallstones (85%) – Radiolucent
Associated with; Fat (metabolic syndrome), Female, Forty, Fertile (estrogenic influence)
The formation is due to disruption in the solubility equilibrium of bile.
- Increased cholesterol secretion into bile.
Old, Obesity/rapid weight loss, Hyperlipidaemia, Increased oestrogens
- Decreased emptying of the gallbladder. GB malignancy, GB hypo-motility, Pregnancy, Fasting/TPN
Pigment stones (15%) – Radio-opaque
- Black (sterile) gallstones. Hard, speculated and brittle.
Composition: Calcium bilirubinate, calcium phosphate and calcium carbonate
Formation due to:
- Increased secretion of bilirubin into bile (e.g. chronic haemolysis, cirrhosis)
- Decreased bilirubin solubilizers and gallbladder stasis
- Brown (infected) gallstones. Soft stones
Composition: Calcium bilirubinate, calcium palmitate, calcium stearate and bacterial cell bodies
Formation due to:
- Infection with bacterial unconjugation of conjugated bilirubin leading to precipitation
- Biliary stasis
Mixed stones
Biliary sludge – Microlithiasis suspended in bile which predisposes to stone formation. 20% disappear, 60% recur, 10% form stones.
CLINICAL PRESENTATION
3 Clinical stages: asymptomatic, symptomatic and complicated cholelithiasis.
Asymptomatic.
Majority of patients (80-95%)
Incidental finding at imaging or laparotomy
Symptomatic gallstones
Biliary colic.
Site –Epigastric (70%) or RUQ, periodicity- distinct attacks lasting 30 mins to several hours often resolving spontaneously, radiation-inferior angle of the right scapula or tip of right shoulder, character- waxing and waning with rarely pain-free intervals, severity-pain is steady and intense, timing- within hours from eating often awakening patient from sleep.
O/E- Positive murphy’s sign
Complicated gallstones
In the gallbladder;
- Acute calculous cholecystitis
- Porcelein GB/ chronic cholecystitis
- GB cancer
- Mirizzi’s syndrome
In the CBD;
Choledocholithiasis leads to:
- Obstructive jaundice
- Ascending cholangitis
- Secondary biliary cirrhosis
- Gallstone pancreatitis
In the GUT;
- Cholecystoenteric fistula
- Bouveret syndrome
- Gallstone dyspepsia
DIAGNOSIS
Through history and P/E and confirmatory imaging studies.
- Plain abdominal x-ray- low pickup rate
- U/S of the hepatobiliary system. Invx of choice
Features include a strong echogenic rim around the stone with posterior acoustic shadowing.
- CT scan. Used to detect complications
- MRCP
- ERCP. The value lies in its therapeutic potential.
- Percutaneous transhepatic cholangiography (PTC)/ biliary drainage (PTBD)
- HIDA Scan. Used in biliary atresia.
TREATMENT
Asymptomatic – Observation
- Keep patient NPO
- Analgesia
- Antibiotics
- Subsequent management. When vitals are stable, oral fluids are reinstated, followed by a regular diet and further imaging. (U/S to confirm dx, MRCP to r/o choledocholithiasis)
Indications for surgery include:
- Patients with chronic haemolytic disease, e.g. SCD, thalassemia
- Diabetic patients
- Patients with a high risk of malignancy
Symptomatic
Cholecystectomy(Treatment of choice) if no medical C/I
Laparoscopic (preferred) or open approach
Non-surgical ways of stone treatment
- Shock-wave lithotripsy
- Medical treatment (Radiolucent gallstones, <15mm, moderate obesity, mild/no symptoms)
- Chemodissolution – Long term oral bile acid ursodeoycholic/ chenodeoxycholic acid
- Liver diet: Moderate carbohydrates, low fat and cholesterol, high fibre.












