
Barrett’s esophagus is a condition in which the normal squamous epithelial lining of the esophagus is replaced by columnar epithelium due to chronic gastroesophageal reflux disease (GERD). This metaplastic change increases the risk of developing esophageal adenocarcinoma.
Epidemiology
- Prevalence: Barrett’s esophagus occurs in approximately 5-15% of patients with chronic GERD and is more common in males than females.
- Age: Most commonly diagnosed in individuals aged 50-70 years.
- Ethnicity: Higher prevalence in Caucasian populations compared to African American or Asian populations.
- Associated Conditions: Obesity, hiatal hernia, and chronic reflux are significant risk factors.
Pathophysiology
The pathophysiological process underlying Barrett’s esophagus involves:
- Chronic Inflammation: Repeated exposure of the esophageal epithelium to acidic gastric contents leads to inflammation and injury.
- Metaplasia: As a protective response, the squamous cells undergo metaplasia, resulting in the transformation to intestinal-type columnar epithelium.
- Dysplasia: Progressive dysplastic changes can occur, leading to low-grade and high-grade dysplasia, which are precursors to esophageal adenocarcinoma.
Classification
- Long-segment Barrett’s Esophagus: Involves ≥3 cm of affected esophageal mucosa.
- Short-segment Barrett’s Esophagus: Involves <3 cm of affected mucosa.
Clinical Presentation
- Symptoms:
- Often asymptomatic; many patients have underlying GERD symptoms (heartburn, regurgitation, dysphagia).
- Possible alarm symptoms indicating complications:
- Unexplained weight loss
- Odynophagia (painful swallowing)
- Anemia or gastrointestinal bleeding (indicating potential malignancy)
- Signs: Physical examination may be unremarkable, but signs of complications like anemia may be present.
Diagnosis
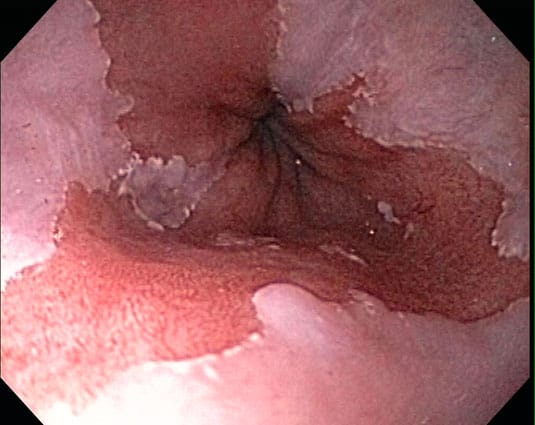
- Endoscopy: The gold standard for diagnosis.
- Procedure: Esophagogastroduodenoscopy (EGD) allows direct visualization of the esophagus.
- Findings: Presence of salmon-colored mucosa above the gastroesophageal junction is characteristic.
- Biopsy: Multiple biopsies (at least four quadrants every 2 cm) should be taken to assess for dysplasia and confirm the diagnosis.
- Histopathological Examination: Biopsy results are classified as follows:
- Non-dysplastic Barrett’s Esophagus: Normal columnar cells without dysplastic changes.
- Low-Grade Dysplasia: Mildly atypical cells present; increased mitotic activity but well-formed glands.
- High-Grade Dysplasia: Significant atypia; loss of architectural organization; considered a precursor to cancer.
- Imaging Studies:
- Barium Swallow: May show a hiatal hernia or esophageal strictures but is not diagnostic for Barrett’s esophagus.
- Endoscopic Ultrasound (EUS): Useful for assessing depth of invasion and regional lymph node involvement if malignancy is suspected.
Management
- Medical Management:
- Proton Pump Inhibitors (PPIs): First-line therapy to control acid reflux.
- Dosage: Omeprazole 20 mg orally once daily, with titration based on symptoms and endoscopic findings.
- Endoscopic Mucosal Resection (EMR): Indicated for visible lesions or dysplastic areas in non-invasive cancer.
- Radiofrequency Ablation (RFA): Considered for patients with high-grade dysplasia or non-dysplastic Barrett’s esophagus to reduce cancer risk.
- Proton Pump Inhibitors (PPIs): First-line therapy to control acid reflux.
- Surgical Management:
- Nissen Fundoplication: Surgical option for refractory GERD and Barrett’s esophagus, particularly in patients with poor PPI response.
- Esophagectomy: Reserved for patients with high-grade dysplasia or early cancer who are surgical candidates.
- Surveillance:
- Regular Endoscopic Surveillance:
- Non-dysplastic Barrett’s: Every 3-5 years.
- Low-grade dysplasia: Every 6-12 months.
- High-grade dysplasia: Every 3 months or sooner, depending on treatment.
- Regular Endoscopic Surveillance:
Complications
- Esophageal Adenocarcinoma: The most significant complication; risk is approximately 30-40 times higher in patients with Barrett’s esophagus compared to the general population.
- Strictures: Can develop due to chronic inflammation or post-therapy changes.
- Perforation: Rare but serious complication during endoscopic procedures.
Prognosis
- Overall Survival: Non-dysplastic Barrett’s esophagus has a good prognosis with appropriate management.
- Cancer Risk: Patients with high-grade dysplasia or early-stage cancer require careful monitoring and management to improve outcomes.












