- Home
- INTERNAL MEDICINE
- Strongyloidiasis

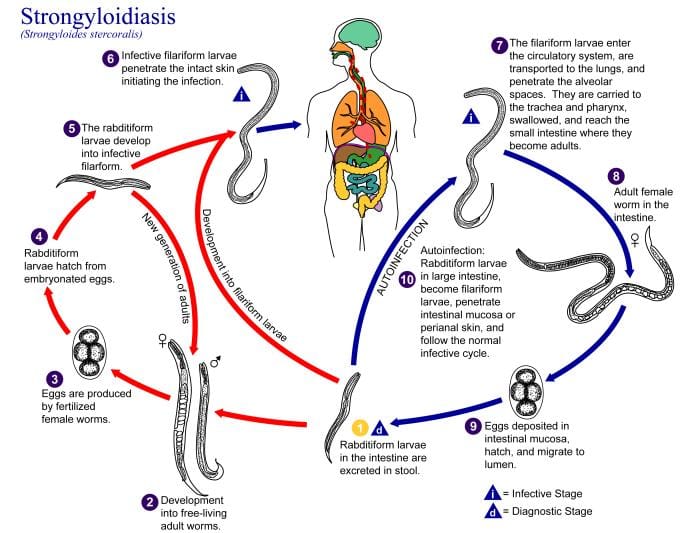
Strongyloidiasis is a helminthic infection caused by Strongyloides stercoralis, a nematode. It is endemic in rural areas. Chronic asymptomatic disease can occur since it can complete its cycle in the human host.
Transmission occurs mainly through skin contact with contaminated soil. Less commonly through the faecal-oral route or person to person. Nosocomial transmission has been reported.
Infection is caused by filariform larvae which migrate to the lungs and get swallowed. The larvae mature into adult worms and burrow into the mucosa of the duodenum and jejunum.
Risk factors for severe disease;
- Impaired cell-mediated immunity, e.g. HIV
- Patients taking steroids
Clinical presentation
- Classical triad- abdominal pain, diarrhoea and urticaria
- Cutaneous phase- pruritus, urticarial tracts, swelling, erythema and a maculopapular rash
- Pulmonary stage- hemoptysis, dry cough, wheezing, pneumonia ( Loeffler syndrome)
- Intestinal phase- nausea, vomiting, diarrhoea and abdominal pain
Severe disease;
Associated with; –
- A massive invasion of the lungs
- CNS involvement
- Gram-negative sepsis
*All systems should be examined
Investigations
- Complete blood count- eosinophilia
- Stool examination for larvae
- Jejunal aspirate and string test- identify the larvae
- Endoscopy-though not used routinely for diagnosis
- Serology- through ELISA, immunofluorescence
- Stool nucleic acid amplification tests- have greater specificity
Differential diagnosis
- Ascariasis
- Ancylostomiasis
- Cutaneous larva migrans
- Meningococcal meningitis
- Ulcerative colitis
Management
- Ivermectin 200mcg/kg on successive days. Alternative: albendazole 15mg/kg bd for 3 days
- Uncomplicated disease- ivermectin alone is adequate
- Severe disease- ivermectin plus empiric antibiotic therapy against enteric gram negatives
- Hyperinfection syndrome- ivermectin 200mcg/ kg for 5 to 7 days
Prevention
- Ivermectin prophylaxis
Complications
- Hyperinfection syndrome can lead to organ dysfunction and septic shock.