- Home
- INTERNAL MEDICINE
- Polycystic Ovarian Syndrome (P ...
Polycystic Ovary Syndrome (PCOS) is a common endocrine disorder affecting women of reproductive age, characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovarian morphology.
It is associated with various metabolic, reproductive, and psychological manifestations. PCOS is a leading cause of infertility and increases the risk for type 2 diabetes mellitus, cardiovascular disease, and endometrial cancer.
Epidemiology
- Prevalence: Affects approximately 6-12% of reproductive-age women, though the prevalence can vary based on diagnostic criteria (Rotterdam, NIH, AE-PCOS Society).
- Risk factors: Genetic predisposition, lifestyle factors (obesity, sedentary behavior), and ethnic background influence the likelihood of developing PCOS.
Pathophysiology
The pathogenesis of PCOS is multifactorial, involving genetic, hormonal, and environmental factors:
- Hyperandrogenism: Elevated levels of androgens (e.g., testosterone, androstenedione) cause hirsutism, acne, and alopecia. Increased ovarian androgen production is often due to elevated luteinizing hormone (LH) levels and insulin resistance.
- Insulin resistance and hyperinsulinemia: Common in PCOS, contributing to hyperandrogenism by enhancing androgen production in the ovaries and reducing sex hormone-binding globulin (SHBG) levels, leading to more bioavailable androgens.
- Ovulatory dysfunction: Characterized by irregular or absent ovulation, resulting in oligomenorrhea or amenorrhea.
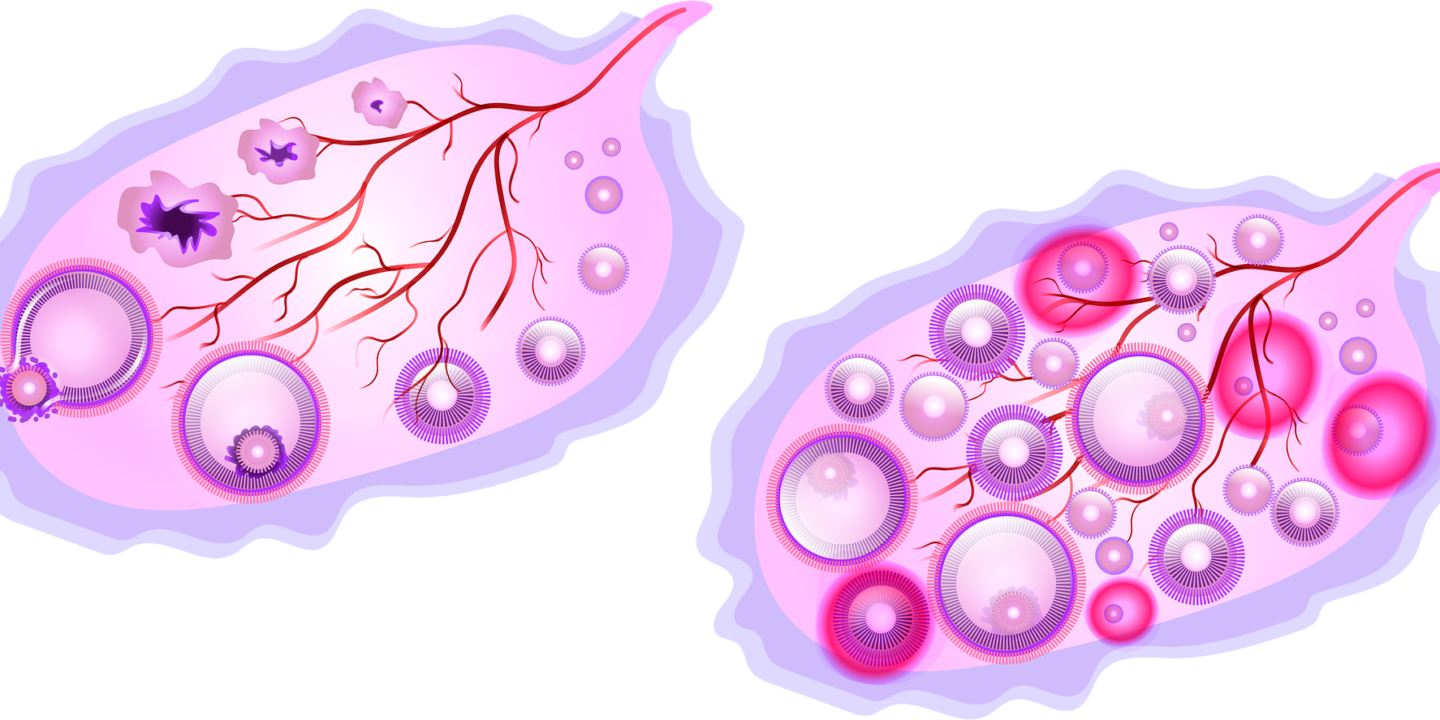
- Polycystic ovarian morphology: The ovaries may appear enlarged with numerous small follicles on ultrasonography, though the presence of polycystic ovaries is not required for diagnosis.
Diagnostic Criteria
The diagnosis of PCOS is established based on the presence of at least two of the following three criteria (Rotterdam criteria):
- Ovulatory dysfunction: Oligo-ovulation or anovulation leading to irregular menstrual cycles.
- Clinical or biochemical hyperandrogenism: Hirsutism, acne, or elevated serum androgen levels.
- Polycystic ovarian morphology on ultrasound: Defined as ≥12 follicles measuring 2–9 mm in diameter or increased ovarian volume (>10 mL) in at least one ovary.
Other potential causes of hyperandrogenism and ovulatory dysfunction, such as congenital adrenal hyperplasia, androgen-secreting tumors, and hyperprolactinemia, should be excluded.
Clinical Manifestations
Reproductive Symptoms:
- Menstrual irregularities: Oligomenorrhea (cycles >35 days) or amenorrhea (absence of menstruation for >3 months).
- Infertility: Resulting from anovulation, making PCOS one of the most common causes of female infertility.
- Hyperandrogenic symptoms: Hirsutism (excessive hair growth in a male pattern), acne, and androgenic alopecia.
Metabolic Features:
- Insulin resistance: Present in 50-70% of women with PCOS, increasing the risk of type 2 diabetes.
- Obesity: Central obesity is common, further exacerbating insulin resistance and metabolic risks.
- Dyslipidemia: Elevated triglycerides and low high-density lipoprotein (HDL) cholesterol.
Psychological Issues:
- Increased prevalence of anxiety, depression, and eating disorders.
- Body image concerns due to weight gain, hirsutism, and acne.
Diagnostic Evaluation
- Laboratory Tests
- Serum testosterone, DHEAS (dehydroepiandrosterone sulfate): To assess for hyperandrogenism.
- Sex hormone-binding globulin (SHBG): Typically reduced in PCOS.
- LH/FSH ratio: Elevated LH to follicle-stimulating hormone (FSH) ratio (>2:1) may support the diagnosis but is not required.
- Fasting glucose, insulin levels, and lipid profile: To assess for insulin resistance and metabolic syndrome.
- Imaging:
- Pelvic ultrasound: To evaluate for polycystic ovarian morphology.
- Exclusion of other conditions:
- Thyroid function tests, prolactin, and 17-hydroxyprogesterone levels to rule out other causes of menstrual irregularities.
Management Strategies
The management of PCOS is individualized, targeting reproductive, metabolic, and dermatologic concerns:
Lifestyle Modifications:
- Weight loss (5-10% of body weight) can improve insulin sensitivity, menstrual regularity, and ovulation.
- Dietary changes: Emphasis on a low glycemic index diet and regular physical activity.
Pharmacological Treatments:
- Oral contraceptive pills (OCPs): First-line therapy for menstrual irregularities and hyperandrogenism. Combined OCPs containing estrogen and progestin help regulate menstrual cycles and reduce hirsutism.
- Dosage: Low-dose OCPs (e.g., ethinyl estradiol 20-35 mcg combined with a progestin) are commonly used.
- Anti-androgens:
- Spironolactone: 50-100 mg orally twice daily to reduce hirsutism and acne. Should be combined with contraception due to teratogenic potential.
- Finasteride: 2.5-5 mg daily may be used for hirsutism, especially if spironolactone is not tolerated.
- Metformin:
- Dosage: 500 mg orally once daily, titrated up to 1,500-2,000 mg/day. Useful for improving insulin sensitivity, weight loss, and ovulatory function.
- Indications: Particularly beneficial in women with metabolic features or those with impaired glucose tolerance.
- Clomiphene citrate:
- Dosage: 50 mg orally daily for five days, starting on day 2-5 of the menstrual cycle. It induces ovulation in women seeking fertility.
- Alternative: Letrozole (2.5-5 mg daily for five days) may be preferred due to a higher ovulation and live birth rate compared to clomiphene.
Fertility Treatments:
- Ovulation induction with clomiphene or letrozole is the first-line treatment.
- Gonadotropin therapy or laparoscopic ovarian drilling can be considered for resistant cases.
- In vitro fertilization (IVF) may be required for persistent infertility despite other interventions.
Management of Dermatological Symptoms:
- Eflornithine cream (13.9%): Applied topically twice daily to reduce facial hair growth.
- Laser hair removal or electrolysis for long-term management of hirsutism.
Psychological Support:
- Counseling for anxiety, depression, and body image concerns.
- Cognitive-behavioral therapy (CBT) for eating disorders if present.
Long-Term Complications and Risk Reduction
- Endometrial hyperplasia and cancer: Due to unopposed estrogen, regular use of progestins (e.g., OCPs or cyclic progestin therapy) is recommended for endometrial protection.
- Cardiovascular disease: Address risk factors like obesity, dyslipidemia, and hypertension.
- Type 2 diabetes: Routine screening for glucose intolerance, particularly in those with risk factors such as obesity and family history.












