- Home
- INTERNAL MEDICINE
- Diabetes Mellitus

Diabetes mellitus (DM) is a group of metabolic disorders characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Chronic hyperglycemia is associated with long-term damage to various organ systems, particularly the eyes, kidneys, nerves, heart, and blood vessels. The two primary forms are Type 1 Diabetes Mellitus (T1DM) and Type 2 Diabetes Mellitus (T2DM), with other specific types such as gestational diabetes mellitus (GDM) and monogenic diabetes.
Pathophysiology
Type 1 Diabetes Mellitus (T1DM):
- T1DM is primarily caused by autoimmune destruction of pancreatic beta-cells, leading to absolute insulin deficiency. The autoimmune process typically involves both humoral and cellular immunity, where islet cell antibodies (ICA), insulin autoantibodies (IAA), and other antibodies such as GAD65 and IA-2 play significant roles.
- Genetic predisposition (e.g., HLA DR3-DQ2, DR4-DQ8) and environmental triggers (e.g., viral infections) contribute to the disease onset. However, the exact etiology remains multifactorial.
- Progressive beta-cell destruction results in an inability to maintain euglycemia, especially after meals, with a progressive loss of basal insulin secretion over time.
Type 2 Diabetes Mellitus (T2DM):
- T2DM is a complex disease involving both insulin resistance and a relative insulin secretory defect.
- Insulin Resistance: Occurs primarily in muscle, liver, and adipose tissues. It is influenced by factors such as obesity, physical inactivity, and genetic predisposition. The accumulation of intramyocellular lipids interferes with insulin signaling pathways, thereby reducing glucose uptake.
- Beta-cell Dysfunction: Progressive decline in beta-cell function results in inadequate insulin response to hyperglycemia. This is often attributed to glucotoxicity, lipotoxicity, and chronic inflammation. Additionally, beta-cell mass reduction due to apoptosis further contributes to disease progression.
- Incretin Effect: In T2DM, there is an impaired incretin effect, mainly due to defective secretion and action of glucagon-like peptide-1 (GLP-1) and gastric inhibitory polypeptide (GIP), which further worsens hyperglycemia.
Clinical Presentation
Classical Symptoms:
- Polyuria, polydipsia, polyphagia, and unintentional weight loss are hallmarks of hyperglycemia.
- Patients may present with fatigue, blurry vision, frequent infections (e.g., urinary tract or skin infections), and poor wound healing.
Acute Complications:
- Diabetic Ketoacidosis (DKA): More common in T1DM, it results from severe insulin deficiency leading to uncontrolled lipolysis and ketone body formation. Symptoms include nausea, vomiting, abdominal pain, Kussmaul breathing, and altered mental status.
- Hyperosmolar Hyperglycemic State (HHS): Seen predominantly in T2DM, characterized by profound hyperglycemia (>600 mg/dL), hyperosmolarity (>320 mOsm/kg), and dehydration without significant ketosis. Neurological symptoms, ranging from lethargy to coma, may occur.
Chronic Complications:
- Microvascular Complications:
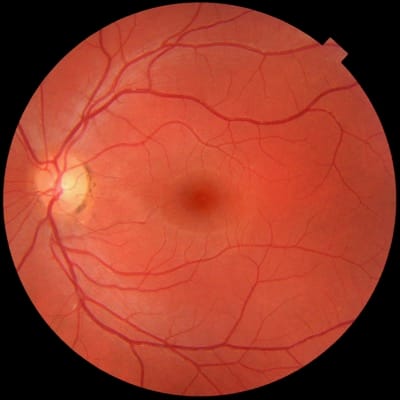
- Diabetic Retinopathy: Leading cause of blindness, classified as non-proliferative or proliferative. Advanced cases may develop macular edema or vitreous hemorrhage.
- Diabetic Nephropathy: Characterized by albuminuria and progressive decline in glomerular filtration rate (GFR). It is the leading cause of end-stage renal disease (ESRD).
- Diabetic Neuropathy: Includes peripheral neuropathy (sensorimotor deficits, pain, or numbness) and autonomic neuropathy (gastroparesis, orthostatic hypotension, erectile dysfunction).
- Macrovascular Complications:
- Cardiovascular Disease (CVD): Diabetic patients have an elevated risk of coronary artery disease (CAD), stroke, and peripheral arterial disease (PAD).
- Lipid Abnormalities: T2DM is associated with an atherogenic lipid profile, characterized by elevated triglycerides, low HDL cholesterol, and small, dense LDL particles.
Diagnostic Criteria
The diagnosis of diabetes mellitus is based on any of the following criteria:
- Fasting Plasma Glucose (FPG) ≥126 mg/dL (7.0 mmol/L).
- 2-hour Plasma Glucose (PG) ≥200 mg/dL (11.1 mmol/L) during a 75g Oral Glucose Tolerance Test (OGTT).
- Hemoglobin A1c (HbA1c) ≥6.5%.
- Random Plasma Glucose ≥200 mg/dL (11.1 mmol/L) with classic symptoms of hyperglycemia or hyperglycemic crisis.
Management
Lifestyle Modification:
- Dietary Recommendations: Emphasize carbohydrate monitoring, prefer low glycemic index foods, increase fiber intake, and limit saturated fat consumption. A Mediterranean or DASH (Dietary Approaches to Stop Hypertension) diet may be beneficial.
- Physical Activity: At least 150 minutes of moderate-intensity aerobic activity per week and resistance training twice a week can improve insulin sensitivity and aid in weight management.
Pharmacological Therapy:
- Oral Antidiabetic Agents:
- Metformin: First-line therapy for T2DM. It decreases hepatic glucose production and improves insulin sensitivity. Gastrointestinal side effects are common.
- Sulfonylureas (e.g., glimepiride, glipizide): Stimulate insulin secretion from beta-cells, but carry a risk of hypoglycemia.
- Thiazolidinediones (e.g., pioglitazone): Improve insulin sensitivity in muscle and adipose tissue but may cause weight gain, fluid retention, and increased risk of heart failure.
- DPP-4 Inhibitors (e.g., sitagliptin): Enhance incretin levels, leading to increased insulin secretion and decreased glucagon secretion.
- SGLT2 Inhibitors (e.g., empagliflozin): Promote renal glucose excretion, which lowers blood glucose. They offer cardiovascular and renal protection but can increase the risk of genital infections.
- Injectable Therapies:
- Insulin Therapy: Necessary for T1DM and indicated in T2DM when oral agents are inadequate. Different regimens include basal-bolus, pre-mixed, or continuous subcutaneous insulin infusion.
- GLP-1 Receptor Agonists (e.g., liraglutide): Improve glycemic control by enhancing insulin secretion, suppressing glucagon, and delaying gastric emptying.
Management of Complications:
- Diabetic Retinopathy: Regular screening and laser therapy for advanced cases.
- Diabetic Nephropathy: Use of ACE inhibitors or ARBs for patients with albuminuria.
- Neuropathy Management: Pain control with agents like pregabalin or gabapentin; preventive care to avoid foot ulcers.
- CVD Prevention: Statin therapy, antihypertensive management, and antiplatelet therapy based on individual risk assessment.
Emerging Therapies and Future Directions
- Cell-based Therapies: Islet cell transplantation and stem cell-based approaches are under investigation for T1DM.
- Artificial Pancreas Systems: Closed-loop insulin delivery systems aim to mimic physiological insulin secretion.
- New Drug Classes: Dual agonists targeting both GLP-1 and GIP receptors, and glucagon receptor antagonists, are promising approaches to improve glucose homeostasis and metabolic control.
- Genomic Medicine: Personalized approaches based on genetic profiling could optimize treatment and improve outcomes.
Effective management of diabetes mellitus requires a multidisciplinary approach, emphasizing early diagnosis, individualized treatment plans, lifestyle modifications, and proactive management of complications. Physicians must remain updated on evolving treatment strategies to optimize patient care and improve quality of life for individuals with diabetes.












