- Home
- INTERNAL MEDICINE
- Renal system
- Benign Prostate Hyperplasia (B ...
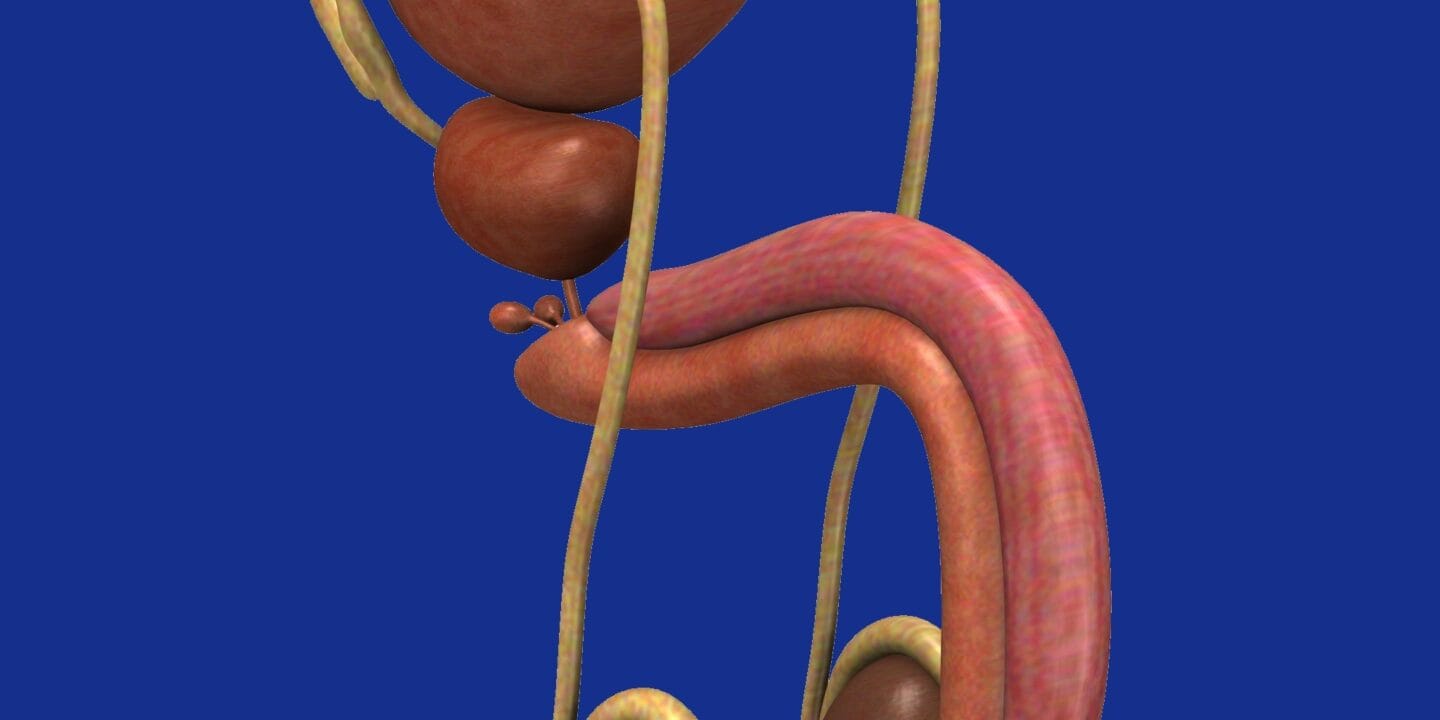
Benign Prostate Hyperplasia is periurethral hyperplasia of stroma and epithelium in the prostatic transitional zone. It affects most men > 50 years but only 10% present with problems.
Aetiology
- Hormonal; DHT required (converted from testosterone by 5 alpha-reductase), the effect of estrogens in increasing expression of DHT receptors.
- Possible role of apoptosis
Clinical Presentation
Symptoms’ severity depends on the degree of encroachment on the prostatic urethra.
- Obstructive symptoms – hesitancy, weak stream, incomplete voiding, terminal dribbling
- Irritative symptoms – frequency, urgency, nocturia, dysuria
- Acute/chronic retention of urine
- Hematuria – From ruptured dilated bladder neck veins.
Complications of obstructive uropathy
- Hydroureter with reflux of urine
- Hydronephrosis
- Pyelonephritis
- UTI
- Nephrolithiasis
- Overflow incontinence
- Hernia secondary to chronic straining
Investigations
- History, assessing lower urinary tract symptoms and impact on QoL. Includes administering IPSS/AUA questionnaire to assess severity.
Scoring: Mild (1-7), Moderate (8-19), Severe (20-35)
- P/E including DRE (prostate smooth and symmetrically enlarged, intact median sulcus, firm consistency with smooth rectal mucosa not attached to prostate)
- FHG: Anaemia, raised WBC due to systemic infection
- UECs: Assess renal function due to chronic obstruction
- U/A to r/o UTI
- PSA to r/o malignancy (Beware of PSA controversy)
- Ultrasonography: Renal, bladder, prostate
- Uroflowmetry. Normal peak flow rate >15ml/s
- Cystoscopy to r/o stones, strictures/bladder neck obstruction or cancer.
Management
Dependent upon the severity of symptoms.
- Watchful waiting
Patients with mild/no symptoms, no complications and normal investigations.
Monitor annually with IPSS scoring, PSA and other invx.
- Medical treatment
- Alpha blockers (Prazosin, Terazosin, Tamsulosin, Alfuzosin)
Relax internal sphincter and smooth muscle of prostate. Take 3 days to be effective.
S/E: Hypotension, Dizziness, Headache, Retrograde ejaculation.
- 5-alpha reductase inhibitors (Finasteride, dutasteride)
Reduce prostate size. Take 3-6 months to be effective.
S/E: Decreased libido, ejaculatory dysfunction, impotence, gynecomastia.
- Anticholinergics – used with caution
- Surgical management
Indications include:
- Failed medical treatment
- Significant complications, e.g. renal insufficiency, recurrent UTI, bladder decompensation.
- Recurrent/persistent gross haematuria
- Bladder calculi secondary to BPH
Methods of performing prostatectomy include:
- Trans-urethral resection of the prostate (TURP) – Minimally invasive.
- Retropubic prostatectomy (Millin’s)
- Transvesical prostatectomy (Freyer’s)
- Perineal approach (Young prostatectomy)
Complications of surgery
- Risks of GA/Spinal anaesthesia
- Bleeding, infection /urosepsis
- Local injury causing incontinence, stricture/bladder neck stenosis
- Retrograde ejaculation
- TUR syndrome
- Failure of procedure/recurrence












