- Home
- GYNECOLOGY/OBSTETRICS
- Obstetrics
- Placenta Previa
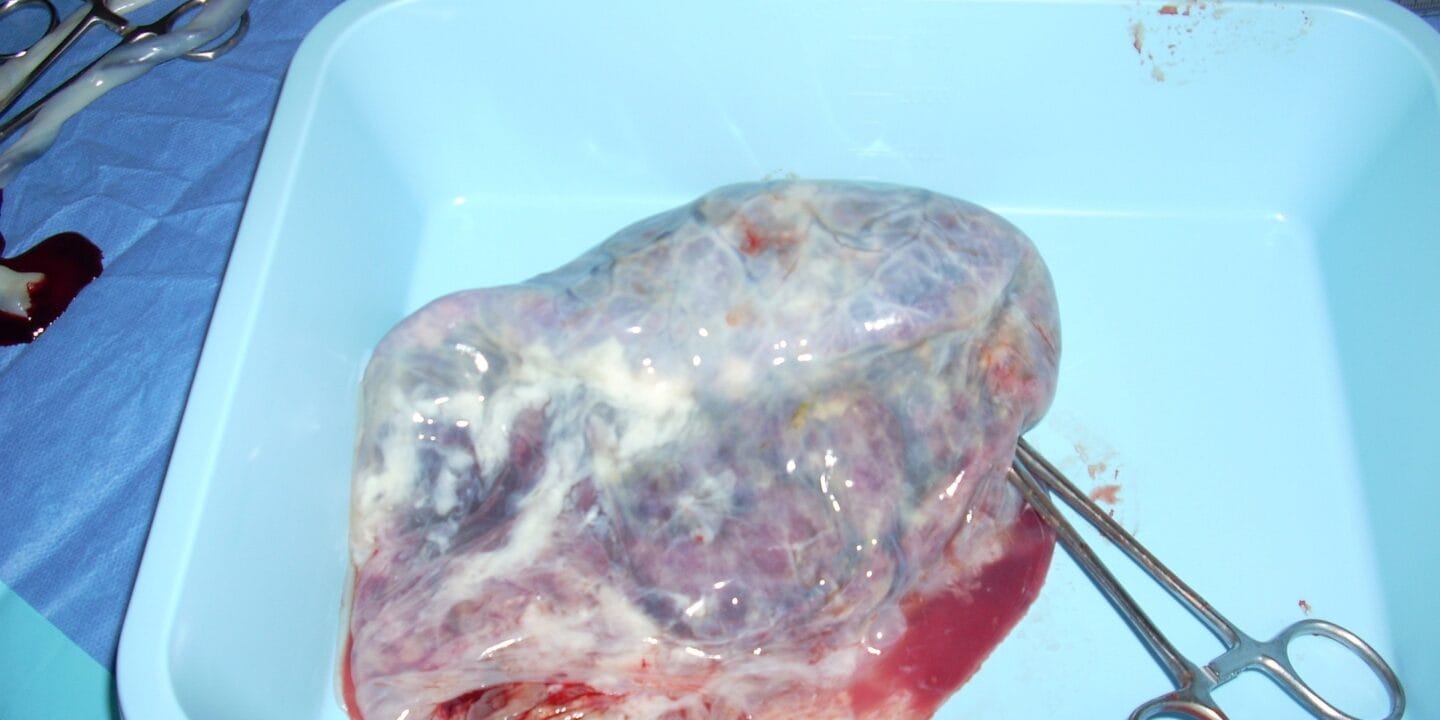
Placenta previa is a condition in which the placenta implants in the lower uterine segment, partially or completely covering the internal cervical os. This condition poses significant risks for both the mother and fetus, particularly during labor and delivery.
Epidemiology
- Incidence: The prevalence of placenta previa is approximately 1 in 200 pregnancies. Its incidence can be higher in women with certain risk factors.
- Risk Factors:
- Previous cesarean deliveries.
- Prior uterine surgery (myomectomy, dilation and curettage).
- Multiparity (having multiple previous pregnancies).
- Advanced maternal age (≥35 years).
- Smoking and cocaine use.
- Multiple gestations (twins, triplets, etc.).
- Previous placenta previa.
Etiology
The exact cause of placenta previa is not fully understood, but several contributing factors have been identified:
- Abnormal Implantation:
- The placenta may implant in the lower uterine segment due to structural changes in the uterus, often related to prior surgical procedures.
- Uterine Anomalies:
- Congenital uterine anomalies (e.g., septate uterus) may influence placentation.
- Inflammation and Scarring:
- History of pelvic inflammatory disease (PID) or endometriosis may lead to scarring and abnormal placental implantation.
Pathophysiology
- Placental Development:
- During normal pregnancy, the placenta typically implants in the upper uterine segment. In placenta previa, the placenta implants in the lower segment, which is not well-vascularized.
- As the uterus expands, the placenta may either partially or completely cover the cervical os.
- Hemorrhage:
- The lower uterine segment is subject to stretching and thinning as the pregnancy progresses. This can lead to potential rupture of placental vessels, causing antepartum hemorrhage.
- The risk of hemorrhage increases with cervical dilation or uterine contractions, particularly during labor.
Clinical Features
- Symptoms:
- Painless Vaginal Bleeding: The hallmark symptom of placenta previa, typically occurring in the third trimester (after 20 weeks gestation). The bleeding can be sudden and may vary in volume.
- Cramping or Uterine Contractions: May be present, especially if associated with labor or preterm labor.
- Signs:
- Abdominal examination may reveal a soft, non-tender uterus.
- Vaginal examination is contraindicated in suspected cases due to the risk of exacerbating bleeding.
Classification
Placenta previa is classified based on the degree of coverage of the internal cervical os:
- Type IV – Complete (Total) Placenta Previa: The placenta completely covers the internal cervical os.
- Type III – Partial Placenta Previa: The placenta partially covers the cervical os.
- Type II – Marginal Placenta Previa: The edge of the placenta is at the margin of the cervical os.
- Type I – Low-Lying Placenta: The placenta is implanted in the lower uterine segment but does not reach the cervical os.
Diagnosis
- Transabdominal Ultrasound:
- Often the initial imaging modality used in suspected cases. It can identify the location of the placenta and assess for any signs of hemorrhage.
- Transvaginal Ultrasound:
- More accurate than transabdominal ultrasound in assessing the position of the placenta relative to the cervical os. It is the gold standard for diagnosis.
- A distance of <2 cm between the placenta and cervical os suggests a higher likelihood of previa.
- MRI:
- In rare cases, MRI may be employed for further evaluation if the ultrasound results are inconclusive or if there are concerns about placental invasion.
- Differential Diagnosis:
- Abruptio placentae.
- Vasa previa.
- Cervical lesions (polyps, tumors).
Management
Antepartum Management
- Hospitalization:
- Hospitalization may be necessary in cases of significant bleeding, depending on gestational age and maternal-fetal stability.
- Activity Modification:
- Bed rest may be recommended, particularly in cases of bleeding.
- Monitoring:
- Close monitoring of maternal vital signs and fetal heart rate.
- Hemoglobin and hematocrit levels should be assessed regularly to evaluate for hemorrhage.
- Corticosteroids:
- Administer corticosteroids (e.g., betamethasone) if preterm delivery is anticipated (typically <34 weeks) to promote fetal lung maturity.
- Avoidance of Vaginal Examinations:
- Vaginal examinations are contraindicated due to the risk of exacerbating bleeding.
Delivery Management
- Timing and Mode of Delivery:
- Delivery is typically planned via cesarean section, especially for complete or partial previa. The timing of cesarean delivery may depend on the degree of bleeding, gestational age, and maternal-fetal status.
- Elective cesarean delivery is usually performed around 36-37 weeks of gestation to minimize the risk of spontaneous labor and bleeding.
- Preparation for Potential Hemorrhage:
- Ensure availability of blood products and IV access for potential massive transfusion.
- Anesthesia Considerations:
- Regional anesthesia (epidural or spinal) is often preferred, but careful assessment is required if significant bleeding is present.
Postpartum Management
- Monitoring for Hemorrhage:
- Close observation for postpartum hemorrhage is essential, as patients with placenta previa are at increased risk.
- Counseling on Future Pregnancies:
- Discuss the potential risks in future pregnancies, including the possibility of recurrent placenta previa or placenta accreta (abnormal placentation).
Complications
- Maternal Complications:
- Severe hemorrhage requiring transfusion.
- Shock and, in rare cases, maternal death.
- Increased risk of cesarean delivery complications (infection, thromboembolism).
- Fetal Complications:
- Preterm birth, often necessitated by maternal bleeding or fetal distress.
- Low birth weight associated with preterm delivery.
- Potential for intrauterine growth restriction (IUGR) due to compromised blood flow.
Prognosis
The prognosis for women with placenta previa depends on several factors, including the degree of previa, the presence of bleeding, gestational age, and maternal health. With appropriate management, most women can achieve favorable outcomes.












