Varicose veins are enlarged, tortuous, and dilated veins that typically occur in the lower extremities due to venous insufficiency. They result from increased venous pressure and valve dysfunction, leading to blood pooling and vein dilation.
Pathophysiology
The development of varicose veins is primarily linked to venous valve incompetence. Normally, the valves within veins prevent blood from flowing backward. When these valves fail or become weakened, blood can pool within the vein, causing increased venous pressure, vein wall stretching, and eventual vein dilation.
Mechanisms Involved
- Venous Valve Dysfunction:
- Primary varicosities: Valve incompetence occurs in the superficial veins without an underlying cause.
- Secondary varicosities: Valve dysfunction results from deep vein thrombosis (DVT), pelvic tumors, arteriovenous fistulas, or congenital abnormalities.
- Venous Hypertension:
- Chronic venous hypertension damages vein walls and valves, perpetuating the cycle of reflux and dilation.
- Vein Wall Changes:
- Structural alterations, including increased collagen and decreased elastin, weaken the vein wall and contribute to venous dilation.
Risk Factors
Several factors increase the risk of developing varicose veins:
- Genetic Predisposition: Family history of varicose veins or chronic venous insufficiency.
- Age: Prevalence increases with age due to weakening vein walls and valve structures.
- Gender: More common in women, possibly due to hormonal influences such as pregnancy and hormonal replacement therapy.
- Pregnancy: Increased venous pressure, hormonal changes (elevated progesterone), and increased blood volume contribute to valve stress.
- Obesity: Excess weight increases pressure in the veins, especially in the lower extremities.
- Prolonged Standing or Sitting: Reduces the effectiveness of the calf muscle pump, which helps propel blood back toward the heart.
Clinical Presentation
Patients with varicose veins may present with:
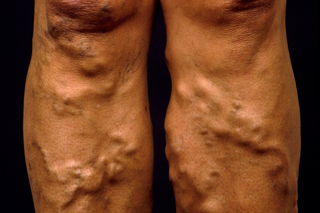
- Visible Dilated Veins: Often bluish, twisted veins that appear just beneath the skin, commonly on the thighs or calves.
- Symptoms:
- Leg heaviness or aching, especially after prolonged standing.
- Leg swelling.
- Skin changes, such as hyperpigmentation or eczema near the affected area.
- Restless legs, particularly at night.
- Superficial thrombophlebitis (inflammation of veins).
- Advanced stages can involve venous ulcers around the ankles.

Diagnostic Evaluation
- Clinical Examination:
- Assess for visible varicose veins, skin changes, and signs of venous insufficiency (e.g., lipodermatosclerosis or venous ulcers).
- Trendelenburg Test: A clinical maneuver used to evaluate the competence of venous valves by having the patient lie down with the leg elevated, followed by rapid standing to see how quickly veins refill.
- Doppler Ultrasound:
- The gold standard for diagnosing venous insufficiency.
- Evaluates valve competence, venous reflux, and deep vein thrombosis.
- Determines the exact location and extent of reflux (e.g., saphenofemoral junction or perforator veins).
- Venography (rarely used):
- An invasive procedure using contrast dye to visualize venous anatomy.
- Indicated in complex cases or before surgical intervention.
Severity Classification
Clinical-Etiology-Anatomy-Pathophysiology (CEAP) Classification is the standardized method used to classify chronic venous disorders:
- C0: No visible or palpable signs of venous disease.
- C1: Telangiectasias or reticular veins.
- C2: Varicose veins.
- C3: Edema.
- C4a: Pigmentation or eczema.
- C4b: Lipodermatosclerosis or atrophie blanche.
- C5: Healed venous ulcer.
- C6: Active venous ulcer.
Management of Varicose Veins
- Conservative Treatment:
- Compression Therapy: Graduated compression stockings help reduce venous pressure, alleviate symptoms, and prevent ulceration. Compression ranges from 20-40 mmHg, based on the severity of venous disease.
- Lifestyle Modifications:
- Weight loss for overweight individuals.
- Leg elevation during rest to reduce venous pressure.
- Regular exercise (e.g., walking, cycling) to enhance the calf muscle pump.
- Medications:
- Venoactive drugs (e.g., diosmin, hesperidin, or rutosides) may alleviate symptoms such as leg pain and heaviness.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for superficial thrombophlebitis.
- Interventional Procedures:
- Sclerotherapy:
- Injection of a sclerosant (e.g., polidocanol, sodium tetradecyl sulfate) into the varicose vein causes endothelial damage, vein fibrosis, and closure.
- Effective for smaller veins (e.g., telangiectasias, reticular veins).
- Endovenous Thermal Ablation:
- Radiofrequency Ablation (RFA): Uses radiofrequency energy to heat and close the incompetent vein.
- Endovenous Laser Therapy (EVLT): A laser fiber inserted into the vein delivers heat to cause vein closure.
- Indicated for larger varicose veins, particularly when associated with saphenous vein incompetence.
- Microsclerotherapy for Spider Veins:
- Injection technique for small superficial veins.
- Often used in cosmetic treatment.
- Sclerotherapy:
- Surgical Treatment:
- Vein Ligation and Stripping:
- Involves tying off and removing the affected saphenous vein.
- Indicated when non-invasive treatments fail or for extensive varicosities.
- Ambulatory Phlebectomy:
- Minimally invasive removal of superficial varicose veins through small skin incisions.
- Vein Ligation and Stripping:
- Emerging Techniques:
- Cyanoacrylate Adhesive:
- Uses medical-grade adhesive to seal the vein.
- A newer, non-thermal, non-tumescent procedure.
- Mechanochemical Ablation (MOCA):
- Combines mechanical irritation with sclerosant infusion to close veins.
- Cyanoacrylate Adhesive:

Complications of Untreated Varicose Veins
- Chronic Venous Insufficiency:
- Persistent venous hypertension leads to skin changes, edema, and ulcers.
- Can progress to lipodermatosclerosis (hardening of the skin and subcutaneous tissues).
- Venous Ulceration:
- Ulcers typically develop near the ankle (medial malleolus).
- Difficult to heal and prone to recurrence.
- Superficial Thrombophlebitis:
- Inflammation and thrombosis of the superficial veins.
- Can be painful and sometimes requires anticoagulant therapy.
- Deep Vein Thrombosis (DVT):
- Risk increases with extensive varicose veins or post-surgical interventions.
Prevention Strategies
- Maintain a Healthy Weight: Reducing body weight alleviates pressure on leg veins.
- Regular Exercise: Physical activity helps promote venous return and prevents blood stasis.
- Avoid Prolonged Standing or Sitting: If unavoidable, frequently change positions or perform calf muscle exercises.
- Use Compression Stockings if at Risk: Especially in those with a family history or occupations involving prolonged standing.












