Diabetic retinopathy is a progressive microvascular complication of diabetes mellitus. It is a leading cause of blindness, with the prevalence increasing with a prolonged duration of diabetes mellitus.
Almost all individuals with type 1 and type 2 diabetes will have some degree of diabetic retinopathy after 20 years.
Pathophysiology
The exact mechanism is unknown, but some theories suggest that
- Hyperglycemia increases retinal blood flow and disrupts intracellular metabolism in retinal endothelial cells and pericytes.
- Vascular autoregulation is impaired, and also increased production of vasoactive substances accompanied by endothelial cell proliferation.
- Decreased capillary hypoperfusion causes chronic retinal ischemia, stimulating the production of growth factors, including vascular endothelial growth factor. (VEGF)
- Vascular endothelial growth factor stimulates deleterious growth of endothelial cells, causing neovascularization and increased vascular permeability causing retinal leakage and exudation.
Risk factors of diabetic retinopathy
- Long-standing duration of diabetes mellitus
- Poor glycemic control
- Hypertension
- Dyslipidemia
- Pregnancy
- Nephropathy/renal disease
- Obesity
- Smoking
Clinical presentation
- There are no early warning signs, but most signs and symptoms are due to complications. They include
- Decreased visual acuity
- Blurred vision
- Floaters
- Flushes
- Visual Field Defects
- Eye pain
- Halos around lights
- Diabetic retinopathy is classified into 2
- Proliferative
- Nonproliferative
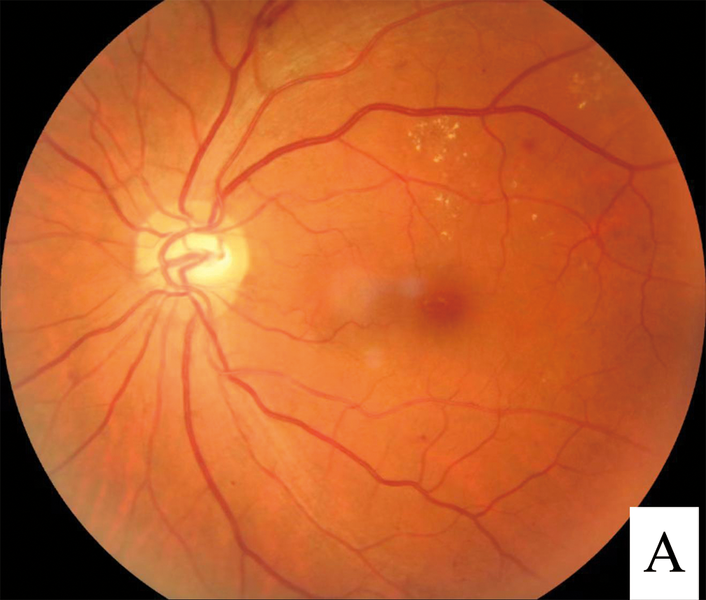
- Nonproliferative is characterized by microaneurysms and retinal hemorrhages. With progression, there are cotton wool spots and venous beading.
- The proliferative stage is characterized by neovascularization.
- Regardless of the stage of diabetic retinopathy, patients may also develop clinically significant macular edema (CSMO). This is the most common cause of vision loss in patients with diabetic retinopathy.
Note: macular edema can cause impairment of visual acuity even if it is associated with only mild peripheral nonproliferative diabetic retinopathy.
- Neovascularization in proliferative diabetic nephropathy can obstruct the eye’s drainage angle and outflow of aqueous flow, causing secondary glaucoma.
- Sudden visual loss in diabetic retinopathy can be a consequence of
- Vitreous hemorrhage
- Retinal detachment
Diagnosis of diabetic retinopathy
Involves
- Systemic workup of diabetes mellitus
- HbA1c-useful for long-term supervision of diabetes mellitus
- OGTT
- Urinalysis detects glycosuria in uncontrolled diabetes and may be useful in detecting proteinuria in diabetic nephropathy.
- Renal function tests
- Random blood sugar
- Fasting blood sugar
- Retinal work up
- Fundoscopy
- Fluorescein angiography-to detect intraregional microvascular abnormalities.
- Ocular ultrasound. Involves B scan ultrasonography which can be used to evaluate the state of the retina in the presence of vitreal hemorrhage.
- Slit lamp retinal bio microscopy-diagnosis of macular edema
- optical coherence tomography. It is used to determine the thickness of the retina and the presence of swelling within the retina, and vitreomacular traction. Particularly used for the diagnosis of macular edema or clinically significant macular edema.
Management of diabetic retinopathy
- Focuses on
- Good glycemic control. Evident by good glycemic targets, including HbA1c of less than 7 %
- Blood pressure control. The target of < 130/80 mmHg is optimal.
- Treatment of dyslipidemia
- Lifestyle changes-exercise, cessation of smoking
These are necessary to prevent the onset and delay the progression of diabetic retinopathy.
- Laser photocoagulation has a role in
- Severe proliferative diabetic retinopathy
- Very severe nonproliferative diabetic retinopathy
- CSMO (clinically significant macula edema)
- Cases of advanced retinopathy due to type 1 diabetes associated with recurrent vitreous hemorrhage causing impaired vision
- Intra vitreal injection
- Anti VEGF/triamcinolone in CSME or proliferative diabetic retinopathy.
- Vitrectomy for tractional retinal detachment threatening the macula
Differential diagnosis of diabetic retinopathy
- Hypertensive retinopathy
- Retinal vein occlusion
- Retinal arterial occlusion
- Coat’s disease
- Retinopathy of prematurity
Complications of diabetic retinopathy
- Retinal detachment
- Macular edema
- Vitreous hemorrhage
- Retinal detachment
- Neovascular glaucoma













