Breast cancer is the 2nd commonest cause of cancer-related deaths in the world.
Pathology
Breast cancer can be invasive or non-invasive. Two major subtypes of lobular and ductal origin include
Non-invasive
- Ductal carcinoma in situ
- Lobular carcinoma in situ
Invasive
- Invasive ductal carcinoma
- Invasive lobular carcinoma
Risk factors
Some of the factors associated with the development of breast cancer include:
- Gender. Females have an increased risk of developing breast cancer compared to women.
- Age. Most common in women with advancing age > 45 years
- Genetic factors-BRCA genes
- Family history of breast cancer and ovarian cancer
- Nulliparity.
- Early menarche
- Late menopause
- Obesity
- Dietary factors-high fat diet and low fibre diet. Diet low in phytoestrogens
- High alcohol intake
- History of previous radiation
- Previous breast cancer
- Hormone replacement therapy
Clinical presentation
Early breast cancer is usually asymptomatic. Most patients develop signs and symptoms of advanced disease.
Patients with signs and symptoms may present as follows
- Painless firm breast lump with ill-defined margins
- The lump is most commonly located in the upper outer quadrant.
- Skin dimpling
- Peau d’orange
- Nipple retraction
- Nipple discharge-blood stained
- Nipple ulceration
- Breast ulceration
Metastatic breast disease can present with
- Axillary and supraclavicular lymphadenopathy
- Bone pain
- Pathologic fractures
- Jaundice
- Abdominal pain
- Abdominal distension
- Nausea and vomiting
- Unintentional weight loss
- Anorexia
- Hemoptysis
- Difficulty in breathing
- Chest pain
- Headaches
- Seizures
- Focal neurological deficits
Differential diagnosis of breast cancer
- TB breast,
- Sarcoma,
- Lymphoma
- Abscess
- Trauma
- Fibro adenoma
- Galactocele
- Cysts
Spread of breast cancer
- Local spread to the skin and chest wall
- Lymphatic spread-axillary lymph nodes
- Haematogenous spread-lungs, liver, bones, brain, peritoneum
Diagnosis of breast cancer
Following a history of clinical presentation of a suspected case of breast ca, breast cancer evaluation is done using Triple assessment, which comprises of
- Clinical assessment
- Imaging-done through ultrasound or mammogram.
Ultrasound for women < 30 years due to higher breast tissue density which makes detection of breast anomalies with mammography very difficult
Mammogram for women greater or equal to 30 years.
- Histopathology and immunohistochemistry, which involve taking fine needle aspiration or core biopsy samples
Other investigations in the workup of a breast cancer patient include
- Complete blood count-may show anemia of chronic disease or as a complication of radio and chemotherapy
- Urea, electrolytes and creatinine
- Liver function tests
- Group and cross matching-useful when there is a need for blood transfusion
- Chest X ray-may show pleural effusions in lung metastases
- Chest CT scan to confirm lung metastases and for staging
- Magnetic resonance imaging-useful in showing metastasis to the brain
- Ct scan chest abdomen to confirm or rule out metastatic breast disease
- Isotope bone scan-for bone metastases
Receptor testing in diagnosed breast cancer
This is necessary to determine the type of receptor expressed in breast cancer biopsy samples, which is crucial for targeted treatment either with hormonal or biological therapy.
Determination of receptor status is done through immunohistochemistry staining.
A tumour can be
- Estrogen receptor positive (ER+) -approximately75% of breast cancers
- Progesterone receptor positive (PR+) approximately65% of breast cancers
- Both estrogen and progesterone receptor positive (ER+, PR+) approximately65% of breast cancers
- Both estrogen and progesterone negative (ER-, PR-), approximately 20% of breast cancers
- Human epidermal growth factor receptor two positive (HER2 +) in approximately 20% of breast cancers
If the breast cancer is negative for estrogen, progesterone, and HER2 receptor, it is referred to as Triple-negative breast cancer. It is highly aggressive and associated with poor prognosis.
Staging of breast cancer
Breast cancer can be staged using
- TNM staging system
- Manchester staging system
TNM staging
| TNM classification | |
| Stage | |
| Tumour size (T) | |
| Tis | Carcinoma in situ. Paget disease of the nipple without underlying invasive carcinoma |
| T1 | Tumour size less than 2 cm |
| T2 | Tumour size 2cm-5cm |
| T3 | Tumour size greater than 5cm |
| T4 | Any tumour size extending to the skin or chest wall |
| Lymph node involvement (N) | |
| N1 | Mobile axillary nodes |
| N2 | Firm axillary nodes |
| N3 | Involvement of supraclavicular lymph nodes |
| Metastasis (M) | |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
Management of breast ca
- Requires multidisciplinary approach as a joint venture between the surgeon, medical
- oncologist, radiotherapists, pathologists, counsellors and nurses
- The basic principles of treatment are to
Reduce the risk of recurrence
Reduce chances of metastatic spread
- Treatment depends on the stage and receptor types of the breast cancer
- Modalities of treatment include :-
Surgery
Chemotherapy
Radiotherapy
Hormonal therapy
Targeted therapy
- Early breast ca stages I & II-surgery and/or radiotherapy
- Stage III –neoadjuvant chemotherapy followed by surgery, then radiotherapy
- Advanced disease stage IV- management supportive
- Palliative care
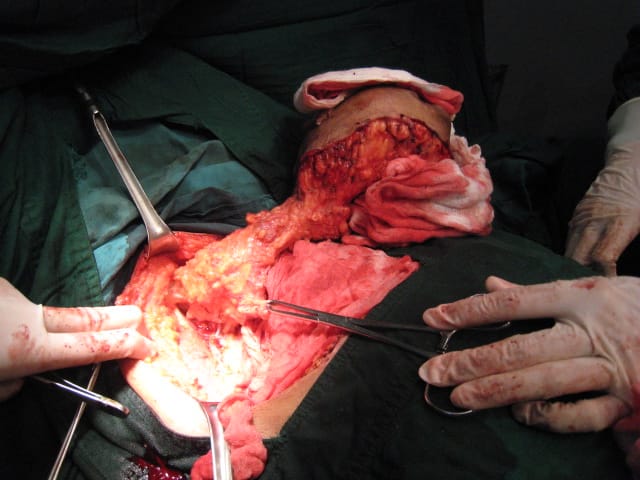
- Toilet mastectomy
- Pain management
- Support nutrition if malnourished
- If ulcerated, regular cleaning and dressing
- Palliative Chemotherapy
- Surgical procedures for breast cancer include
- Breast conservation surgery. Focuses on the removal of the affected breast tissue only :-
Lumpectomy
Partial mastectomy
Quadrantectomy
- Simple mastectomy-removal of the entire breast
- Modified Radical mastectomy-simple mastectomy + ALND (axillary lymph node dissection)
- Toilet mastectomy for inoperable breast cancer to reduce infection, pain, and bleeding.
- Sentinel lymph node Biopsy-in patients with clinically negative node disease
- Mammoplasty
Breast Reduction
Breast Augmentation using implants and Muscles flaps
- Hormone therapy. In patients who have ER/PR-positive tumours. Contraindicated in pregnancy
- Trastuzumab-administered in HER2 receptor-positive breast cancer. Also contraindicated in pregnancy
- Triple-negative breast cancer treated by chemotherapy
Complications of breast cancer
Malignant pleural effusions
Paraneoplastic syndromes
Secondary malignancies to
Complications related to treatment
- Injury to the long thoracic nerve
- Winged scapula
- Arm lymphedema
- Injury /thrombosis of the axillary vein
Prognosis of breast cancer
Prognostic factors include
- Stage of cancer. Early stages have a better prognosis compared to advanced stages.
- Histological Grade. High-grade tumours have a poor prognosis
- Receptor status
Hormone-negative breast cancer has an unfavourable prognosis.
HER2-positive tumours are highly aggressive and hence have a poor prognosis.
Triple-negative breast cancer is a high-grade tumour, highly aggressive, with a poor outcome.
- Early intervention. Has a favourable outcome
- Age. Advanced age associated with poor prognosis
Prevention of breast cancer
- Avoid avoidable risk factors
- Encourage breastfeeding. Breastfeeding is protective
- Health education
- Population screening-
History-risk factors
Cbe-clinical breast exam
Bse-breast self-exam
- Chemo prevention with Prophylactic anti estrogens
- Early diagnosis and early treatment
- Prophylactic bilateral mastectomy and salpingo-oophorectomy in high-risk patients
Screening modalities for breast cancer
- Mammogram
- Ultrasound












