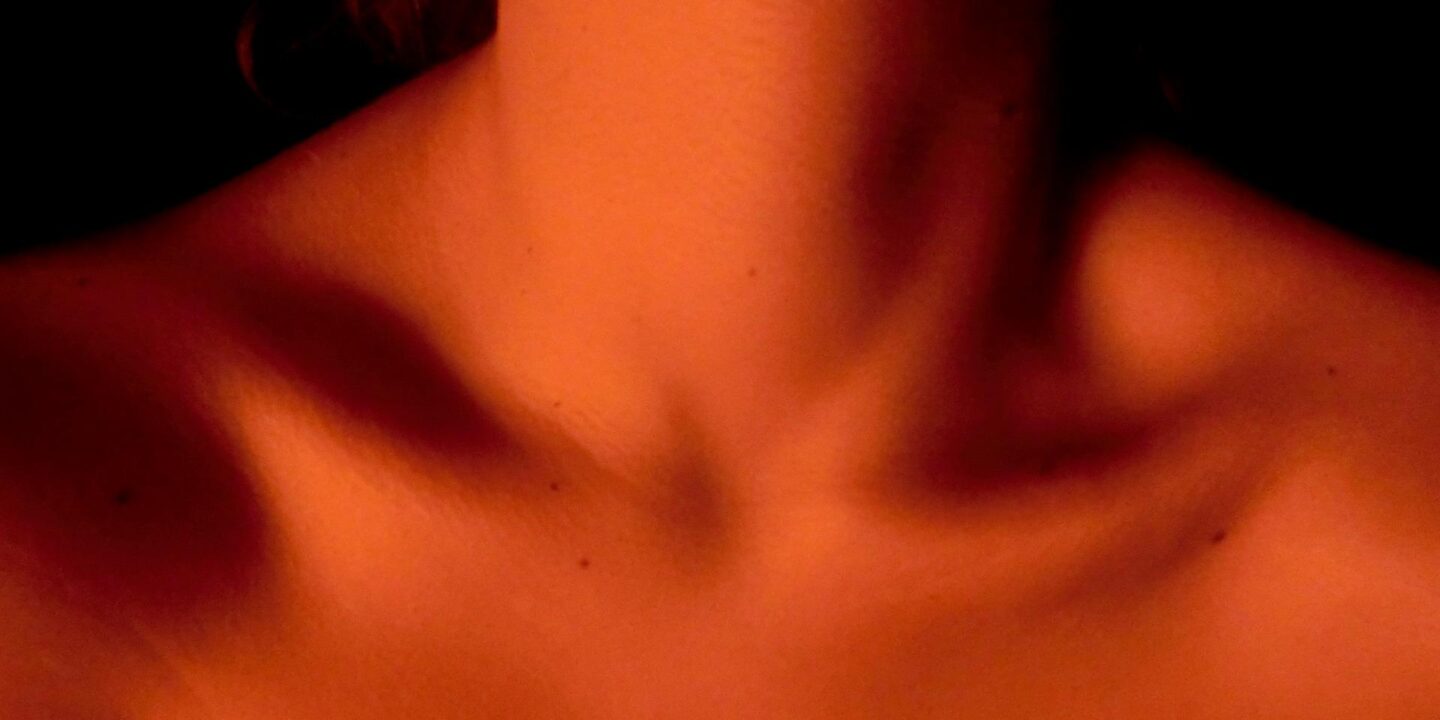
Subacute thyroiditis, also known as De Quervain’s thyroiditis, is a self-limiting inflammatory disorder of the thyroid gland characterized by neck pain, tenderness, and often a triphasic clinical course involving hyperthyroidism, hypothyroidism, and eventual return to euthyroid state. It is believed to be triggered by a viral infection or a post-viral inflammatory response.
Epidemiology
- Incidence: Subacute thyroiditis is relatively rare, affecting approximately 5-6 per 100,000 individuals annually.
- Age and Gender: It predominantly affects women between the ages of 30 and 50, with a female-to-male ratio of about 4:1.
- Seasonal Variation: Cases often increase during outbreaks of viral illnesses, such as mumps, Coxsackie virus, adenovirus, and influenza.
Etiology
- Viral Infections: The condition is often preceded by an upper respiratory tract infection, supporting the hypothesis of a viral etiology.
- Autoimmune Mechanisms: Though not primarily autoimmune, there is an inflammatory immune response in the thyroid, potentially due to viral antigens.
Pathophysiology
- Inflammation of the Thyroid Gland: The viral infection or post-viral inflammatory response leads to granulomatous inflammation of the thyroid tissue.
- Release of Thyroid Hormones: The inflammation causes the release of preformed thyroid hormones (T3 and T4) from damaged follicular cells, resulting in transient hyperthyroidism.
- Resolution and Healing:
- The inflammation subsides over time, and thyroid hormone levels may fall below normal, causing transient hypothyroidism.
- Eventually, the gland recovers, and thyroid function returns to normal.
Clinical Presentation
The presentation of subacute thyroiditis often follows three stages:
Hyperthyroid Phase (Acute Phase):
- Symptoms: Fever, fatigue, weight loss, anxiety, palpitations, and increased sweating.
- Neck Pain: Tenderness over the thyroid gland, which may radiate to the jaw, ears, or chest.
- Duration: Usually lasts 3-6 weeks.
Hypothyroid Phase:
- Symptoms: Fatigue, weight gain, dry skin, constipation, and cold intolerance.
- Duration: Lasts 4-6 weeks.
Recovery Phase (Euthyroid Phase):
- The thyroid gradually returns to normal function.
- Complete resolution of symptoms occurs in most cases within 6-12 months.
Diagnosis
Clinical Evaluation:
- History of recent viral illness.
- Thyroid gland tenderness and neck pain on physical examination.
Laboratory Investigations:
- Thyroid Function Tests:
- Hyperthyroid Phase: Elevated serum T3 and T4, suppressed TSH.
- Hypothyroid Phase: Low T3 and T4, elevated TSH.
- Recovery Phase: Normalization of thyroid hormone levels.
- Erythrocyte Sedimentation Rate (ESR) or C-reactive Protein (CRP):
- Both are typically elevated, reflecting an inflammatory process.
- Thyroid Autoantibodies: Usually absent, helping differentiate from autoimmune thyroiditis (e.g., Hashimoto’s or Graves’ disease).
Imaging Studies:
- Thyroid Ultrasonography:
- Shows a diffusely enlarged and hypoechoic (inflammatory) thyroid gland.
- Radioactive Iodine Uptake (RAIU):
- Low uptake during the hyperthyroid phase, which is a key differentiating factor from Graves’ disease (which shows high uptake).
Differential Diagnosis
- Graves’ Disease: Presents with hyperthyroidism but is differentiated by high RAIU and presence of thyroid-stimulating immunoglobulins (TSIs).
- Hashimoto’s Thyroiditis: Typically presents with a firm, non-tender thyroid gland and positive thyroid autoantibodies.
- Acute Suppurative Thyroiditis: An infection of the thyroid, often with marked systemic symptoms (fever, chills) and bacterial source identification.
- Thyroid Nodules or Cancers: Thyroid cancer rarely causes pain unless there is rapid growth or hemorrhage into a nodule.
Treatment
Symptomatic Management:
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs):
- For pain relief and to reduce inflammation. Common choices include ibuprofen or aspirin.
- Corticosteroids:
- Prednisone may be used for severe cases or when NSAIDs are ineffective. Start with 40-60 mg/day, then gradually taper over 6-8 weeks.
Thyroid Function Management:
- Beta-Blockers (e.g., propranolol or atenolol):
- Used to control symptoms of hyperthyroidism such as palpitations, anxiety, or tremors.
- Thyroid Hormone Replacement:
- Levothyroxine may be required if the patient enters the hypothyroid phase and experiences symptomatic hypothyroidism.
- Treatment is typically temporary, as the thyroid function usually recovers.
Monitoring:
- Regular Thyroid Function Tests: To assess the course of the disease and guide treatment adjustments.
- Symptom Monitoring: To ensure resolution and detect any persistent or recurrent symptoms.
Prognosis
- Self-Limiting Condition: Most patients recover completely within 6-12 months.
- Recurrence: Rare, but some individuals may experience relapses.
- Permanent Hypothyroidism: Occurs in a small percentage of patients, requiring lifelong thyroid hormone replacement.
Complications
- Prolonged Hypothyroidism: Some patients may not fully recover thyroid function.
- Thyroid Storm (Rare): An exaggerated hyperthyroid state with severe symptoms, more common if there is coexisting Graves’ disease.
Prevention
There are no specific preventive measures for subacute thyroiditis, as it is often related to viral infections. General infection control and immune health measures may help reduce the risk.













