- Home
- INTERNAL MEDICINE
- Respiratory system
- Community-Acquired Pneumonia
Pneumonia is defined as an acute infection of the lung parenchyma. It is the most common cause of death in industrialized countries.
It can be classified according to;
1. Location of acquisition- community-acquired or hospital-acquired
2. Etiology-
- viral or bacterial
- Primary or secondary
3. Clinical presentation- typical or atypical
4. Area of lung affected by the disease- lobar; bronchopneumonia; interstitial; cryptogenic
COMMUNITY-ACQUIRED PNEUMONIA
Common at the extremes of age; but can occur in any age group
Spread; most cases are spread via respiratory droplets
Factors predisposing to pneumonia
- Old age
- Cigarette smoking
- Alcohol use
- Glucocorticoid therapy
- Upper respiratory tract infections
- Recent influenza infection
- Pre-existing lung disease
- HIV
- Indoor air pollution
- DM
- Altered consciousness
- Dysphagia
- Toxins, e.g. gasoline
- Crowded living conditions
Microbiology
Streptococcus pneumoniae remains the leading cause.
The age and clinical setting affect the likelihood of a specific organism being the infecting agent
- Mycoplasma– young people
- H. influenzae– in the elderly, especially those with underlying lung disease
- Legionella pneumophila– in local outbreaks
- Staphylococcus aureus– following an influenza episode.
- Klebsiella spp– in alcoholics
Certain occupations are also associated with particular bacteria
Viruses include- influenza, parainfluenza, herpes simplex, varicella, adenovirus, CMV, coronaviruses
Pathophysiology
Failure of pulmonary protective mechanisms, e.g. cough, leads to infiltration of the lung parenchyma by the infecting pathogen. Inflammation occurs, leading to impaired alveolar ventilation and, thus, hypoxia. An abscess may be formed.
Four stages;
- Congestion- days 1 to 2
- Red hepatization- days 3 to 4
- Grey hepatization- days 5 to 7
- Resolution- day 8 to week 4
Clinical presentation
- Usually presents acutely
- Fever, rigours, shivering, malaise, anorexia and headache may be present
- Pulmonale symptoms- dry cough initially followed by a productive cough with mucopurulent sputum( yellow-greenish)
- Rust-coloured sputum for S.pneumoniae
- Hemoptysis may be reported
- Pleuritic chest pain, referred to the shoulder, may be present
- Upper abdominal tenderness in lower lobar pneumonia
Physical exam;
- Pay attention to the respiratory system, pulse, blood pressure and mental status.
- Chest signs depend on the stage of the infection.
- In consolidations, there’s a dull percussion note, bronchial breathing and whispering pectoriloquy on auscultation; crackles are heard throughout
- Herpes labialis points to a streptococcal infection
*Atypical pneumonia- dry cough, non-remarkable auscultation, dyspnoea, headache, malaise, myalgias and sore throat
Investigations
1. Blood;
- CBC- leucocytosis or leucopenia; hemolytic anaemia in Mycoplasma
- Urea and electrolytes- uremia; hyponatremia
- ESR/CRP- elevated
- Blood culture- bacteremia
- LFT- hypoalbuminemia
- Blood gas analysis- may show acidosis
2. Sputum- for culture, gram stain and antimicrobial sensitivity
3. Urine- for pneumococcal or Legionella antigen
4. Oropharyngeal swab- PCR for Mycoplasma
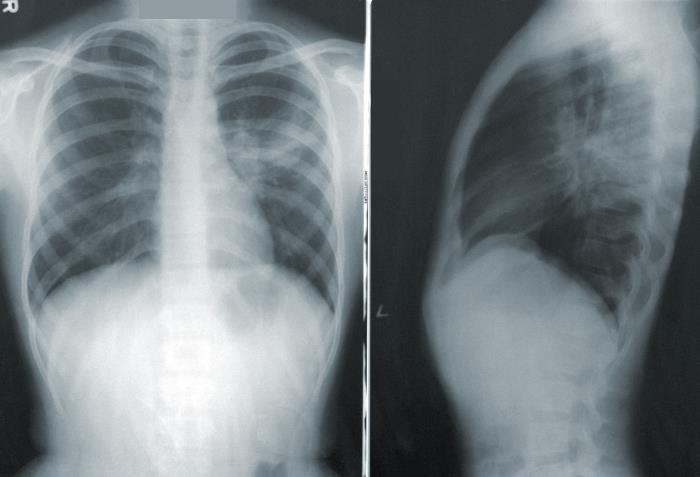
5. Chest Xray-
- Lobar pneumonia- consolidation of the affected lobe, bronchograms
- Bronchopneumonia- patchy and segmental shadowing
- Complications- pleural effusion, abscess
- Staphylococcus aureus- multilobar shadowing, cavitation, abscess
6. Pleural fluid- for culture
Hospital CURB-65 score
- C- confusion
- U- uremia>7 mmol/l
- R- respiratory rate>30/ minute
- B- systolic blood pressure<90 mmHg or diastolic <60mmHg
- Age- >65
Each scores 1 point
Management
1. Oxygen therapy- for all patients with tachypnea, hypotension or acidosis, or SpO2 of less than 92%
- Consider CPAP in those who continue being hypoxic. Consider transfer to an HDU unit.
2. Fluid balance- IV fluids in those with severe disease, in the elderly and those vomiting
- Ensure adequate oral intake for the rest
3. Antibiotics
- The initial choice is guided by severity, local disease patterns and resistance, and clinical context
- In uncomplicated pneumonia, a five-day course is adequate
- Longer treatment in Klebsiella, s.aureus or LegionellaLegionella pneumonia
- Parenteral treatment; in severe illness, impaired consciousness, loss of swallowing reflex, and malabsorption
-Low severity- amoxicillin; doxycycline if allergic to penicillins
-Moderate severity-moderate to high dose amoxicillin or benzylpenicillin plus clarithromycin; alternatively, doxycycline, levofloxacin
-Severe- co-amoxiclav or ceftriaxone plus clarithromycin or benzylpenicillin plus levofloxacin
-Levofloxacin, if Legionella is suspected
4. Analgesia for pleural pain
5. Physiotherapy- assists in expectoration
Complications
- Pleural effusion
- Abscess
- Pneumothorax
- VTE
- Lobar collapse
- ARDS
- Arrhythmias, etc
Prevention
- Cessation of smoking
- Influenza and pneumococcal vaccination
- Public health control in legionella pneumonia
- Immunization against measles, influenza, and pertussis in children
- Reduce indoor pollution and tackling of malnourishment.












