- Home
- GYNECOLOGY/OBSTETRICS
- Cervical Cancer
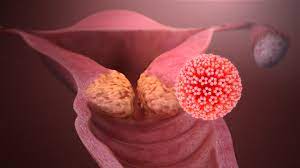
Cervical cancer is caused by long-term infection with human papillomavirus (HPV) and is a significant global health issue.
Ranks fourth in both incidence and cancer-related mortality among women, with over 500,000 new cases and about 300,000 deaths annually.
Incidence
- Cervical cancer accounts for 13.1% of all new female cancers worldwide.
- In Kenya, cervical cancer contributes to 12.9% of new cancer cases annually and 11.84% of all cancer deaths. It is the leading cause of cancer-related deaths in Kenya and the second most common cancer among females.
- In Eastern Africa, it is the most common cancer among women, with an age-standardized incidence and mortality rate of 40.1 and 30.0 per 100,000, respectively.
- The World Health Organization (WHO) estimates that there are over 1 million women globally who have cervical cancer and do not have access to the necessary health services for prevention, treatment, or palliative care.
Risk factors for cervical cancer
- Infection by the human papillomavirus
- Becoming sexually active at a young age
- Having many sexual partners
- Having one partner who is considered high-risk (someone with HPV infection or who has many sexual partners)
- History of smoking.
- Having a weakened immune system eg in the case of HIV/AIDS
- History of chlamydia infection
- Long-term use of oral contraceptives (birth control pills)
- Having multiple full-term pregnancies
- Young age at first full-term pregnancy
- Having a family history of cervical cancer
- Use of Diethylstibestrol (DES)
Clinical presentation
Cervical cancer is often asymptomatic in the early stages. Here are the most common presenting symptoms.
- Abnormal vaginal bleeding (e.g., post-coital, intermenstrual, or post-menopausal)
- Vaginal discharge
- Dyspareunia
- Pelvic pain
- Weight loss
Diagnosis of Cervical Cancer
Screening of cervical cancer
Screening programs play a crucial role in the early detection and treatment of cervical cancer, which can significantly impact its prevention.
When precancerous lesions are detected through screening, they can easily be treated, preventing the development of cancer. Screening can also detect cancer in its early stages, allowing for effective treatment.
Despite the availability of HPV vaccination for girls, which can reduce the risk of developing cervical cancer later in life, regular screening is still necessary for older women
According to Kenya’s guidelines, screening tests include:
- HPV DNA testing is recommended as the primary screening method for women above 30 years of age.
- Where HPV testing is not yet available, or loss-to-follow-up is a risk, then Visual Inspection with Acetic acid (VIA) or Visual Inspection with Acetic acid and Visual Inspection with Lugol’s iodine (VIA/VILI) is recommended as the primary screening method
- Pap smear is recommended as a primary screening method in the following situations:
- For women not eligible for VIA or VIA/VILI because their squamo-columnar junction (SCJ) is not visible, and HPV screening not accessible
- As a primary test in women under 30 years of age
- As a co-test with HPV in HIV positive women where the resources are available
HPV testing should primarily be conducted in women over the age of 30 years. Testing women younger than 30 years old is not recommended because many young women are infected with HPV which will clear up on their own by the age of 30.
This can result in a high number of false positive results, leading to unnecessary procedures and putting a strain on the healthcare system, with little impact on the incidence of cervical cancer.
thedoctab
If cervical cancer is suspected, a colposcopic examination is done. A unique magnifying instrument (colposcope) is used to check for abnormal cells.
During the colposcopic examination, a sample of the cervical cells (biopsy) is obtained for laboratory testing. To obtain tissue, the doctor may use:
- Punch biopsy involves using a sharp tool to pinch off small cervical tissue samples.
- Endocervical curettage uses a small, spoon-shaped instrument (curet) or a thin brush to scrape a tissue sample from the cervix.
- The electrical wire loop uses thin, low-voltage electrified wire to obtain a small tissue sample.
- Cone biopsy (conization) is a procedure that allows the doctor to obtain deeper layers of cervical cells for laboratory testing.
Staging
Stage 0: Carcinoma in situ (CIN 111).
Stage 1:
Carcinoma confined to the cervix.
La: Preclinical carcinoma that is diagnosed only by microscopy.
La 1: Stromal invasion no greater than 3mm and no wider than 7mm (so-called Micro-invasive carcinoma)
La 2: Maximum depth of invasion of stroma greater than 3mm and no greater than 5mm taken from the base of epithelium, either surface or glandular from which it originates, horizontal invasion, not more than 7mm.
Lb: Histologically invasive carcinoma confined to the cervix and greater than stage la2.
Stage 2:
Carcinoma extends beyond the cervix but not onto the pelvic wall.
Carcinoma involves the vagina but not the lower third.
Stage 3:
Carcinoma has extended onto the pelvic wall.
On rectal examination, there is no cancer-free space between the tumor and pelvicwall.
The tumor involves the lower third of the vagina.
Stage 4:
Carcinoma has extended beyond the true pelvis or involved the bladder or rectum mucosa.
Treatment of cervical cancer
Treatment depends on the stage of the disease. Treatment modalities include:
Surgery
- Cryotherapy – an ablative form of treatment for precancerous lesions of the cervix which freezes cells using a cryoprobe.
- Loop Electrosurgical Excision Procedure
- Cold knife Conisation
- Thermocoagulation
- Surgery to remove the cervix (trachelectomy)
- Surgery to remove the cervix and uterus (hysterectomy)
Radiotherapy
Uses powered energy beams, such as X-rays or protons, to kill cancer cells
Chemotherapy
A drug treatment that uses chemicals to kill cancer cells.
If untreated, death occurs in 95% of cases within 2 years after onset of symptoms.
Causes of death includes
- Hemorrhage (excessive Bleeding)
- -Sepsis(infection)
- Lung complication (pulmonary embolism)
- Ureamia
Prevention of cervical cancer
Several measures can help reduce the chances of developing cervical cancer.
- Human papillomavirus (HPV) vaccine
- Practicing safe sex
- Regular cervical screening
- Having fewer sexual partners
- Delaying first sexual intercourse
- Stopping smoking












