- Home
- INTERNAL MEDICINE
- Empyema
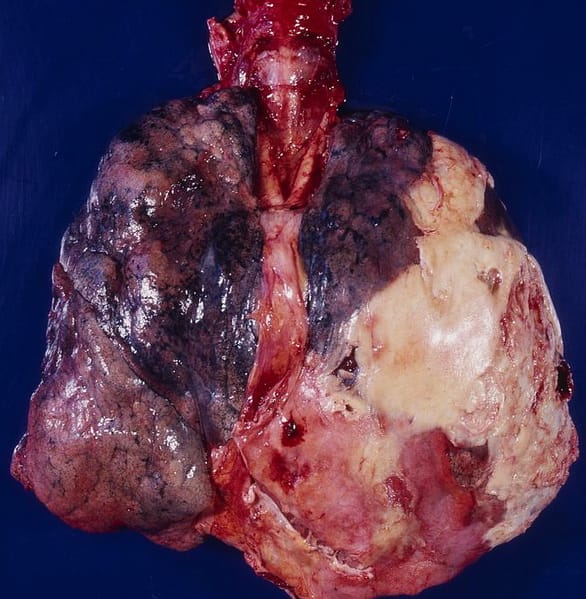
Empyema, also known as pyothorax or pleural empyema, is a collection of pus within the pleural cavity resulting from infection. It is typically associated with pneumonia but can also arise due to trauma, surgery, or underlying lung conditions.
Pathophysiology:
Empyema develops in three stages:
- Exudative Phase: The initial stage involves the accumulation of sterile fluid in the pleural space, characterized by a high protein content and low cellularity.
- Fibrinopurulent Phase: As the infection progresses, bacteria and white blood cells infiltrate the pleural fluid, leading to pus formation. Fibrin deposition occurs, resulting in loculated fluid collections.
- Organizing Phase: Fibroblast proliferation leads to thick pleural peel formation, which may trap the lung and impair re-expansion, potentially causing chronic empyema.
Etiology:
Empyema often results from:
- Bacterial pneumonia (most common): Streptococcus pneumoniae, Staphylococcus aureus, including Methicillin-resistant Staphylococcus aureus (MRSA), and Gram-negative organisms such as Klebsiella pneumoniae.
- Post-surgical infections: Following thoracic surgeries.
- Trauma: Penetrating chest injuries can introduce pathogens into the pleural space.
- Esophageal rupture (Boerhaave syndrome) or diaphragmatic hernia.
- Intra-abdominal infections: Transdiaphragmatic spread.
Risk factors include underlying chronic lung diseases, immunosuppression, diabetes, alcoholism, and age extremes.
Clinical Presentation:
Patients may present with:
- Symptoms: Fever, pleuritic chest pain, dyspnea, cough (productive or non-productive), and systemic signs of sepsis. Symptoms may have an insidious onset, especially in chronic cases.
- Physical Examination: Decreased breath sounds, dullness to percussion, and decreased tactile fremitus on the affected side. Pleural friction rub may be present.
Diagnostic Approach:
- Imaging Studies:
- Chest X-ray: Shows pleural fluid collection with blunting of the costophrenic angle. In lateral decubitus views, fluid layers suggest free-flowing effusion.
- Chest CT Scan: Preferred for identifying loculated fluid collections, pleural thickening, and underlying lung pathology. Helps guide drainage procedures.
- Ultrasound: Useful for identifying fluid pockets for thoracentesis.
- Pleural Fluid Analysis:
- Diagnostic Thoracentesis: Essential for confirming empyema. Pleural fluid typically shows:
- pH < 7.2
- Glucose < 40 mg/dL
- Elevated lactate dehydrogenase (LDH), often >1000 IU/L
- Polymorphonuclear leukocytes predominance
- Microbiological Studies: Culture, Gram stain, and PCR for specific pathogens.
- Diagnostic Thoracentesis: Essential for confirming empyema. Pleural fluid typically shows:
- Laboratory Tests:
- Complete blood count (CBC): Leukocytosis may indicate infection.
- Inflammatory markers: Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
Management:
Treatment is based on the stage of empyema, clinical status, and underlying cause.
- Antibiotic Therapy:
- Empiric coverage should target common pathogens, including Streptococcus spp., Staphylococcus aureus, and Gram-negative organisms.
- Initial Empiric Therapy: Intravenous (IV) antibiotics such as:
- Ceftriaxone (2g IV once daily) + Metronidazole (500mg IV every 8 hours) for anaerobic coverage.
- Piperacillin-tazobactam (4.5g IV every 6 hours) for broader coverage.
- In cases of suspected MRSA: Vancomycin (15-20 mg/kg IV every 8-12 hours), aiming for a trough level of 15-20 µg/mL.
- Duration of Therapy: Generally 3-4 weeks, tailored based on clinical response and radiological improvement.
- Drainage Procedures:
- Thoracentesis: Effective for early-stage, free-flowing effusions.
- Chest Tube Insertion (Tube Thoracostomy): Required for loculated or fibrinopurulent empyema. Use of a small-bore catheter (10-14 Fr) may be considered, though larger-bore catheters (20-28 Fr) may be necessary for thick pus.
- Intrapleural Fibrinolytic Therapy: Recombinant tissue plasminogen activator (tPA) plus deoxyribonuclease (DNase) (e.g., tPA 10 mg + DNase 5 mg intrapleurally twice daily for 3 days) may be used to break down loculations.
- Surgical Intervention:
- Video-Assisted Thoracoscopic Surgery (VATS): Indicated for patients with failure of drainage and fibrinolytic therapy. Allows for decortication and removal of the thick pleural peel.
- Open Thoracotomy with Decortication: Considered in chronic empyema where thick fibroelastic tissue entraps the lung.
- Open Window Thoracostomy: An option for debilitated patients where definitive surgery poses a high risk.
Post-Treatment Monitoring and Complications:
- Serial imaging (chest X-rays or CT scans) is essential to monitor resolution.
- Pulmonary function tests may be indicated to assess lung recovery post-resolution.
- Potential complications include bronchopleural fistula, fibrothorax, and lung entrapment.
Chronic Empyema Considerations:
- Chronic empyema is defined by the persistence of symptoms or radiologic findings beyond 3 weeks.
- Management may involve a combination of long-term antibiotics, repeated drainage, and possibly, surgery.
- The approach should be multidisciplinary, involving pulmonologists, infectious disease specialists, and thoracic surgeons.
Prognosis:
- The prognosis largely depends on prompt diagnosis, the severity of the infection, the presence of comorbidities, and timely intervention.
- Mortality rates can be significant in cases with advanced sepsis, delayed treatment, or in patients with underlying immunosuppression.












